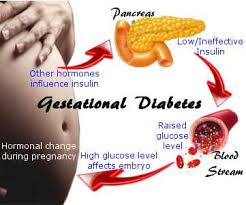
Gestational diabetes arises in certain women who cannot overcome the insulin resistance that develops during pregnancy. In most cases, the condition goes away after the baby is delivered. However, women who have gestational diabetes have increased risks of developing Type 2 diabetes later in life.
It’s important to note that gestational diabetes is not actually the cause of that long-term increased risk of Type 2 diabetes. In fact, it’s the other way around: the increased risk of Type 2 diabetes was there all along, even before pregnancy, and is the cause of the gestational diabetes.
“Gestational diabetes appears to be an early symptom of an abnormal ability to secrete insulin,” explains Dr. Lorraine Lipscombe, director of the Centre for Integrated Diabetes Care at Women’s College Hospital (WCH). “It’s an early sign of a disorder that can eventually lead to Type 2 diabetes.”
Insulin, a hormone secreted by the pancreas, regulates blood sugar levels. Abnormal insulin secretion can lead to high blood sugar, which is the main characteristic of diabetes.
Treatment for gestational diabetes protects the baby from the effects of high blood sugar and from the increased insulin production required to control it. Because insulin is a growth factor, women with gestational diabetes may have large babies, which increases the risk of delivery complications. The increased need for insulin can also stress the baby’s pancreas before birth.
“There is evidence emerging that if they are exposed to high blood sugars in pregnancy, the baby’s pancreas has to work harder and that can lead to a potential increased risk of diabetes and insulin secretory defects in the baby,” Dr. Lipscombe explains. “That’s the other concern: that over the years it predisposes the baby to a higher risk of Type 2 diabetes, so it’s a vicious cycle.”
Early warning
Gestational diabetes is treated in pregnancy to try to avoid or minimize the short- and long-term risks to the baby. For mothers, it can provide an early warning of their own health risks.
“Women get gestational diabetes because they have risk factors for Type 2 diabetes, but it hasn’t developed yet,” Dr. Lipscombe says. “As they get older, especially if they gain weight or if they have an unhealthy diet, or they have other factors that play into the increased challenge to the pancreas, then eventually the pancreas has to work harder, and eventually it fails to the point where they get Type 2 diabetes.”
While it may increase the baby’s future diabetes risk, research indicates that gestational diabetes does not add to a woman’s pre-existing risk of Type 2 diabetes.
“A number of studies have compared women who do and do not get pregnant, who have similar risk profiles,” Dr. Lipscombe says. “One group will get gestational diabetes in pregnancy and the other group won’t get it because they never got pregnant. And it appears that the pregnancy does not increase the risk further. So the gestational diabetes does not make them progress to Type 2 diabetes more rapidly.”
Although the lifetime risk of Type 2 diabetes for women with gestational diabetes may be as high as 50 per cent, it is not a certainty. Research suggests that lifestyle can play an important role in managing those risks for women who have had gestational diabetes.
Research using data from the Nurses’ Health Study II looked at the long-term health of study participants with a history of gestational diabetes.
“For the women who remained more active and kept their weight healthy, their risk of diabetes was much lower despite the gestational diabetes,” Dr. Lipscombe says. “So we know that by keeping to a healthy weight and staying physically active you can reduce your risk of Type 2 diabetes even if you had gestational diabetes. It’s not a fait accompli – you can do something about it.”
Encouraging healthy changes
That’s one of the reasons Dr. Lipscombe and her colleagues at the Women’s College Hospital Research Institute are studying a preventive program. Now in its pilot phase, it is designed to support new mothers who have had gestational diabetes to make healthy lifestyle changes. The home-based program is adapted from WCH’s highly successful Women’s Cardiovascular Health Initiative program. It includes telephone counselling and a personal health coach to help women build healthier habits to reduce their long-term risk of Type 2 diabetes.
“It’s not easy to engage new mothers to change their behaviour when they’ve just had a baby,” Dr. Lipscombe says. “We’ve trained the coaches to be sensitive to the fact that these women are in a very demanding period of their life, but it is a time when bad habits do form because of those challenges.”
There is no data from the trial yet, but it has completed recruitment. Dr. Lipscombe reports that they have received positive feedback from participants: 98 per cent would recommend the program to other mothers with gestational diabetes, and 96 per cent described their own experience in the study as good, very good or excellent.
“We’ve had over 70 women who have come back for their final assessment and many have really made positive changes and were starting to see positive results,” she says. “It’s our hope that they will sustain that long-term.”







