Pregnancy is a beautiful phase of every women's life; with little precaution this journey can be memorable. Hellodox wishes happy nine months with expert advice on yoga, exercise, meal plans, natural care and home care. Get the best pregnancy care tips and charts on HelloDox.
Pregnancy can put quite a strain on your body. As your body changes to accommodate the growing baby, you may find yourself suffering from a few common discomforts associated with the various stages of pregnancy. Most of these are nothing to worry about. Here are a few of the most common problems faced by pregnant women.
Backaches: As the body’s ligaments stretch and become softer to prepare for labour, you may feel a strain on your lower back and pelvis. This can cause a chronic backache. The growing weight of the fetus within your body can also add to this discomfort.
Morning sickness: Despite its name, morning sickness can affect you at any time of the day. Most women begin to experience nausea and an urge to vomit from the 4th or 6th week of pregnancy, but this usually resolves itself by the 16th or 20th week of pregnancy. Some women may even feel sick for the entire day.
Bleeding gums: Pregnancy hormones can make your gums more vulnerable to the build-up of plaque. This can lead to inflammation and bleeding gums. This condition may also be known as pregnancy gingivitis.
Cramps: Many pregnant women complain of cramps in their calves and feet. This usually is more common at night, but the cause behind it is not clear.
Urinary incontinence: Urinary incontinence is a problem experienced by many women during and after pregnancy. They often find themselves involuntarily urinating while coughing, laughing or sneezing. In most cases, this is a temporary problem caused by the relaxation of pelvic floor muscles (to prepare for delivery) and should resolve itself after delivery. Women may also find themselves feeling the urge to urinate frequently. This may be because of the pressure being placed on your bladder by the uterus.
Skin and hair changes: Pregnancy hormones can make birthmarks, moles and freckles darken. Your nipples may also turn darker. In addition to this, you may notice the bumps around the nipples become more prominent. Pregnant women may also find their skin more prone to sunburns. You may also notice an increased rate of hair growth.
Feeling hotter than normal: The hormonal changes occurring during pregnancy can make you feel warmer than normal because of increased blood supply to the skin. You may also find yourself sweating more than usual. In addition, you may also feel faint because of decreased blood supply to the brain.
One of the most important aspects of staying healthy is to keep your body hydrated by drinking enough water. When it comes to drinking water, we stress on purifying it but do you ever stop to think about how you are storing your water? The vessel in which water is stored in not only contains it but also interacts with it and influences the chemical elements in it. In the old days, water was stored in earthen matkas but today, water bottles have become more popular. These bottles are commonly made of glass or plastic both of which can be harmful in the long run. Instead, Ayurveda suggests the use of copper vessels to store water. Here are a few reasons for this.
Plastic vs Glass vs Copper
One of the chemical elements present in all plastic bottles is Bisphenol A or BPA. This chemical has been linked to a number of diseases including cancer. They also contain a number of other toxins that are gradually absorbed by the water inside the bottle. Exposure to BPA when pregnant can lead to a woman giving birth to an underweight baby. This chemical can also affect the development of the brain and behaviour. Disposable mineral water bottles should never be reused for this reason. Plastic bottles also absorb odors and tend to leak after repeated use.
The glass is an inert material and hence when used to store water, does not influence it in any way. The two things you should look for, if you choose to buy glass bottles is that they are lead and cadmium free. However, glass bottles are not cheap and have a tendency to crack or break. Once broken, these bottles cannot be reused.
Copper also influences the chemical balance in the water. However, this does not harm the body in any way, but in fact, has a number of benefits. Copper acts as a natural sterilizer and has an oligodynamic effect on water stored in it. It has the ability to destroy a number of harmful pathogens that are commonly found in water. Copper is an element needed by the body and drinking water stored in a copper vessel supplies our body’s daily copper requirement.
Copper can also help regulate cholesterol, heart rate and blood pressure levels. Copper has also been associated with an ability to regulate thyroid functioning, ease joint pains, improve fertility, heal internal wounds, help in hemoglobin synthesis and in maintaining the proper acid-alkaline balance in our bodies. A copper bottle may seem a little expensive when you buy it but there is no chance of breakage. Hence, if handled properly, a copper bottle can last a lifetime.
From the given arguments it is clear that using a copper vessel is the best way to store water.
October is the start of flu season. It’s also the time of year when people have questions about flu shots and flu prevention. To clear up some common concerns, here are some of the most common myths about flu shots, along with the facts.
Myth: You can get the flu from the flu shot.
Fact: This is simply not true. In fact, it’s impossible.
“It is not a live vaccine,” explains Alexis Valente, interim manager of occupational health, safety and wellness at Women’s College Hospital. “You cannot get the flu from the flu shot because it is an inactive virus that is in the shot.”
Even though the vaccine used in flu shot injections contains no live vaccine, this is one of the most common myths about flu shots. Some people report that they became ill after having the shot, but they had probably already been exposed to whatever made them ill.
“It’s likely because something was already in their system, but they weren’t showing symptoms yet,” Valente says. It takes about two weeks for the flu vaccine to take effect, so people are still at risk immediately after getting a shot. That’s one of the reasons people are encouraged to get their flu shot early.
Myth: I don’t need a flu shot because I got one last year.
Fact: To be protected, you need to get a flu shot every year.
There are two reasons for this. One is that a flu shot’s protection wears off over time. The second is that the flu virus changes – or mutates – over time. The vaccine is updated from one year to the next, to try to make it as effective as possible against the current flu virus.
“There are different strains of flu virus,” Valente says. “So each year a new vaccine is formulated based on research predicting which viruses are likely to be common this season.”
Myth: The flu shot is not effective.
Fact: The flu shot does not always provide complete protection, but it is the best protection available.
There are different strains of flu virus, and the vaccine does not protect against all of them. Effectiveness can vary from year to year depending on how accurately the vaccine matches the strains that are circulating that year.
“Last year, for the 2015-16 flu season, the flu shot was 64 per cent effective,” Valente says. “That’s not as high as some other years. However, it’s better than being zero per cent effective if you don’t get a flu shot.”
Myth: I eat well and exercise, so I won’t get the flu.
Fact: Anyone can catch the flu.
That’s why the flu shot is recommended for most people over six months old. A healthy lifestyle is very important to your overall well-being and long-term health, but flu shots and good hand hygiene are the best defence against flu.
The flu virus spreads through droplets that are transported when an infected person coughs, sneezes or talks. People nearby can inhale these droplets and become infected. Infected people can also leave droplets on surfaces such as doorknobs, elevator buttons, or other surfaces that many people touch. Another person can become infected by touching these surfaces and then touching their own nose, mouth or eyes. That’s why it’s so important to clean your hands frequently and use hand sanitizer.
“Two things we really promote here at Women’s College Hospital are good hand hygiene and getting a flu shot, because in healthcare the rate of getting flu is much higher than in other workplaces,” Valente says.
Myth: The flu is no big deal.
Fact: Flu can be a serious illness.
Valente notes that complications that can arise from flu include pneumonia, hospitalization and, in rare cases, even death.
According to the Public Health Agency of Canada, there are about 1 billion cases of flu worldwide every year, and 3 million to 5 million of those cause severe illness. The flu kills between 250,000 and 500,000 people worldwide every year. The most vulnerable groups include people over age 65 or under age 5, pregnant women, and people with other health conditions.
Even in cases that don’t become severe or life-threatening, the flu is very unpleasant and usually lasts 10 days to two weeks.
Another thing to consider is the possibility of passing the flu virus to someone more vulnerable.
“You can pass it on to a family member, a colleague or a member of the public,” Valente says.
Myth: Pregnant women should not get a flu shot.
Fact: Canada’s National Advisory Committee on Immunization (NACI) notes that pregnant women are at increased risk for complications from flu, and recommends flu shots for all pregnant women.
Flu shots by injection are safe in pregnancy. In fact, NACI notes that vaccinating pregnant women protects against flu in their newborns (who cannot be vaccinated against flu until age six months).
“It’s recommended for pregnant women regardless of the stage of pregnancy,” Valente says. “And also for those who are breastfeeding, and those who are planning a pregnancy.”

Women who need treatment for depression or anxiety while pregnant may find reassurance in a new study. The new research found no increased risk of autism associated with using antidepressant medication during pregnancy.
The study’s key findings include:
Use of selective serotonin reuptake inhibitors (SSRIs) in pregnancy was not independently associated with greater risk of autism in children.
In women who had taken SSRI antidepressants during one pregnancy and not in another, there was no difference in autism risk between the siblings.
There was no difference in autism risk between children whose mothers took SSRI antidepressants in pregnancy, and children whose mothers stopped taking antidepressants shortly before pregnancy.
The study was published in JAMA on April 18, 2017, and included 35,906 births in Ontario from 2002 to 2010. The results may help women make decisions about treatment for depression or anxiety while pregnant.
“There is a great deal of pressure on women not to take medications during pregnancy,” says study author Dr. Simone Vigod, a psychiatrist at Women’s College Hospital. She notes that while it is important to weigh the risks and benefits of any medication, it’s also important to consider the effects of not treating a condition.
“I think people fail to consider that untreated mental illness in pregnancy can have serious impact,” she says.
Some of the risks of untreated depression or anxiety in pregnancy include:
Effects on the baby either directly through the illness itself, or through symptoms like poor sleep or poor nutrition that can affect the fetus.
The longer mental illness is untreated, the harder it can be to treat, and the higher the risk of chronic mental illness.
It may have a negative impact on the woman’s relationships with her partner and her other children.
The biggest risk factor for postpartum mental illness is untreated mental illness during pregnancy.
The study counters earlier research that suggested a possible link between antidepressant use in pregnancy and autism risk in children. Dr. Vigod says the new research used a more detailed approach to ensure an accurate comparison.
“The problem with those earlier studies is that for women who take antidepressant medications during pregnancy, there’s some reason why they’re taking the medication: they suffer from depression or anxiety,” she says.
That alone means there may be differences between these women and those not taking antidepressants, so a simple comparison of autism rates may be very misleading.
“It’s possible that depression or anxiety could have a direct impact on fetal brain development through physiological mechanisms,” Dr. Vigod explains. “It has been shown that depression and autism have a shared genetic predisposition. So if a woman has depression or anxiety, even if she’s not symptomatic in pregnancy, her child might have a higher risk of developing autism just by shared genetics.”
The symptoms of anxiety and depression may also have an effect on pregnancy.
“For example, if a woman has depression or anxiety she may also be more likely to not have as good nutrition, she might not be sleeping as well, she might be more likely to use alcohol or drugs, or she might have other medical conditions.”
All of those issues make it hard to isolate the possible effects of antidepressant medications from the potential effects of mental illness.
“We set out to try to balance out the groups to better understand whether this was a causal relationship or not,” Dr. Vigod says.
More accurate comparisons
To do that, she and her research colleagues used a special method called high dimensional propensity score (HDPS) analysis. This method looks for thousands of different types of health claims, from diagnoses and prescriptions to hospital stays and emergency department visits. The HDPS score of the women who took antidepressants in pregnancy was then matched to a more balanced group of women with a similar score, but who did not take antidepressants in pregnancy.
“When we did that in our main analysis, suddenly there was no longer an association between antidepressant exposure and autism,” Dr. Vigod says.
The researchers then looked at some of the results more closely.
First, they identified women who had at least two children, and who had taken antidepressants in at least one pregnancy and not in another. They compared autism risk in the siblings, and found no difference between the children exposed to antidepressants and those who weren’t.
Then, they compared the children of women who took antidepressants in pregnancy to the children of women who stopped taking antidepressants shortly before pregnancy.
“Again, in that analysis those children were not significantly different in their autism risk,” Dr. Vigod says.
These additional comparisons support the main study result: the findings showed no evidence that antidepressants in pregnancy are independently related to autism risk in children.
“What that suggests is that while kids whose moms took antidepressants may be at higher risk of autism, it’s probably not because of the antidepressants,” Dr. Vigod says.
“While we can never say that any medication exposure has zero risk, in general these medications are relatively low risk, so if women require them for their psychiatric stability, they can feel reassured that they are not unduly putting their children at risk.”
The study results may also be reassuring to mothers of children with autism who may have used antidepressants during pregnancy.
“These results may also be reassuring for those parents, to say that your child having autism isn’t a result of a decision you made,” Dr. Vigod says. “I think that can be very helpful, too.”
While women are having more children today than they were 10 years ago, according to the Pew Research Center, they're also having babies when they're older — a recent report found that 86% of U.S. females have given birth between the ages of 40 and 44, a 6% increase from 2006.
That may be why fertility is also a common issue, as the Office on Women's Health says one of the top risk factors concerning an inability to conceive is age. So it begs the question: When is a woman the most fertile?
The Facts About Fertility
Your odds of getting pregnant are highest in your 20s and 30s, as this is when women are technically the most fertile and have some of the best quality eggs, says Beth W. Rackow, M.D., associate professor of obstetrics and gynecology and pediatrics at Columbia University Medical Center. It's also when you're least likely to have to wait: According to the American College of Obstetricians and Gynecologists (ACOG), healthy couples in their 20s and 30s have a 25-30% chance of getting pregnant in a single menstrual cycle.
But around age 35, those numbers slowly and steadily dwindle, Dr. Rackow says. The risk of miscarriage also increases due to poorer egg quality. After age 37, a woman's odds of becoming pregnant decreases rapidly, ACOG says, and by the time a woman celebrates her 40th birthday, there's a less than 10% chance of getting pregnant within each menstrual cycle.
Which is why, if a woman is under the age of 35 and has been trying to get pregnant for one year, it's recommended that she receive an infertility evaluation, Dr. Rackow says. If she's between the ages of 35 and 40, only wait six months before seeing a specialist. In your 40s, it's important to seek medical attention if there are no signs of conception after only two or three cycles.
"We don't want to scare women that by age 35 they aren't going to get pregnant — that's not the case," Dr. Rackow says. "[But] it gets more difficult as a woman gets older, so we don't want them, at age 35, to be trying for two years and then see us when we could have done something sooner."
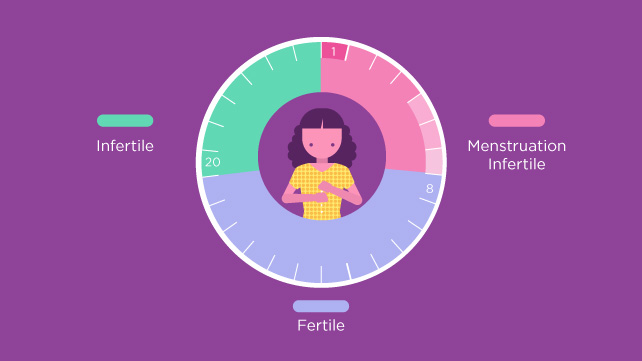
Your Fertility During Each Cycle
Making a baby the old-fashioned way comes down to figuring out when your body is ovulating. The ovulation phase, or the time in a woman's menstrual cycle in which an ovary releases an egg in order to be fertilized, lasts up to two days. There's the day of ovulation itself (AKA when the egg is released), along with the 24 hours leading up to it. That's when you're most fertile, Dr. Rackow says.
Couple that with sperm's ability to live inside the female reproductive tract for 48 to 72 hours, and your highest likelihood of success is, you guessed it, during the ovulation phase. "We encourage couples to be intimate every other day leading up to the timing of ovulation, and then every day [during the ovulation phase]," Dr. Rackow says.
As for how to pinpoint this momentous monthly occurrence, begin by tracking the length of your menstrual cycle, as some women's cycles can be 26 days and others' 32 (though the average is 28), Dr. Rackow says. Then, pay attention to when you get your period. "About 12 to 14 days before your next period is usually when you would ovulate," she says.
Your body also gives signs that you're ovulating. Clear vaginal discharge (or cervical mucus), breast tenderness, and pelvic cramping are common symptoms, Dr. Rackow says, and many women also experience a slight increase in body temperature during the ovulation phase, according to the American Pregnancy Association.
How to Tell When You're Ovulating
Other than reading the all-natural signs from your body, there are ways to tell if you're ovulating. Dr. Rackow recommends a urine ovulation kit, which measures when the body has a surge of luteinizing horrmone that signals ovulation. And while there are digital tests available, she notes that the daily test strips work just as well.
Pregmate 50 Ovulation LH Test Strips
$15.95
BUY NOW
Otherwise, a fertility app could be useful in helping you keep track of your cycle. That way you always have it on you, you can log symptoms on the fly, and you can even set up alerts to remind you when you're in the ovulation phase. (And tell your partner it's time to get busy.) Nathaniel DeNicola, M.D., assistant professor of obstetrics and gynecology at the GW School of Medicine and Health Sciences, says the ones he sees being used most frequently are Glow, Clue, and Ovia Health (formerly known as Ovuline).
Just don't rely on the apps to be the end-all, be-all source of knowledge for getting pregnant. Yes, health apps are on the rise — a recent study found that more than 70% of U.S. adults use an app to self-monitor their well-being — but Dr. DeNicola says the limited research that has been conducted to determine the accuracy of predicting the fertility window “has been a little underwhelming.”
And, whatever you do, don't forget to tell your doctor about any tests and trackers you're using when trying to conceive, Dr. DeNicola says. "A lot of what we do in fertility and achieving conception counseling is looking at the timing of periods," so your doctor will be able to use that information to get a more in-depth look at your health, potentially making it easier to spot health concerns, notice if something is irregular, or make more personalized suggestions that could result in fertility success.