One of the most important aspects of staying healthy is to keep your body hydrated by drinking enough water. When it comes to drinking water, we stress on purifying it but do you ever stop to think about how you are storing your water? The vessel in which water is stored in not only contains it but also interacts with it and influences the chemical elements in it. In the old days, water was stored in earthen matkas but today, water bottles have become more popular. These bottles are commonly made of glass or plastic both of which can be harmful in the long run. Instead, Ayurveda suggests the use of copper vessels to store water. Here are a few reasons for this.
Plastic vs Glass vs Copper
One of the chemical elements present in all plastic bottles is Bisphenol A or BPA. This chemical has been linked to a number of diseases including cancer. They also contain a number of other toxins that are gradually absorbed by the water inside the bottle. Exposure to BPA when pregnant can lead to a woman giving birth to an underweight baby. This chemical can also affect the development of the brain and behaviour. Disposable mineral water bottles should never be reused for this reason. Plastic bottles also absorb odors and tend to leak after repeated use.
The glass is an inert material and hence when used to store water, does not influence it in any way. The two things you should look for, if you choose to buy glass bottles is that they are lead and cadmium free. However, glass bottles are not cheap and have a tendency to crack or break. Once broken, these bottles cannot be reused.
Copper also influences the chemical balance in the water. However, this does not harm the body in any way, but in fact, has a number of benefits. Copper acts as a natural sterilizer and has an oligodynamic effect on water stored in it. It has the ability to destroy a number of harmful pathogens that are commonly found in water. Copper is an element needed by the body and drinking water stored in a copper vessel supplies our body’s daily copper requirement.
Copper can also help regulate cholesterol, heart rate and blood pressure levels. Copper has also been associated with an ability to regulate thyroid functioning, ease joint pains, improve fertility, heal internal wounds, help in hemoglobin synthesis and in maintaining the proper acid-alkaline balance in our bodies. A copper bottle may seem a little expensive when you buy it but there is no chance of breakage. Hence, if handled properly, a copper bottle can last a lifetime.
From the given arguments it is clear that using a copper vessel is the best way to store water.

Women who need treatment for depression or anxiety while pregnant may find reassurance in a new study. The new research found no increased risk of autism associated with using antidepressant medication during pregnancy.
The study’s key findings include:
Use of selective serotonin reuptake inhibitors (SSRIs) in pregnancy was not independently associated with greater risk of autism in children.
In women who had taken SSRI antidepressants during one pregnancy and not in another, there was no difference in autism risk between the siblings.
There was no difference in autism risk between children whose mothers took SSRI antidepressants in pregnancy, and children whose mothers stopped taking antidepressants shortly before pregnancy.
The study was published in JAMA on April 18, 2017, and included 35,906 births in Ontario from 2002 to 2010. The results may help women make decisions about treatment for depression or anxiety while pregnant.
“There is a great deal of pressure on women not to take medications during pregnancy,” says study author Dr. Simone Vigod, a psychiatrist at Women’s College Hospital. She notes that while it is important to weigh the risks and benefits of any medication, it’s also important to consider the effects of not treating a condition.
“I think people fail to consider that untreated mental illness in pregnancy can have serious impact,” she says.
Some of the risks of untreated depression or anxiety in pregnancy include:
Effects on the baby either directly through the illness itself, or through symptoms like poor sleep or poor nutrition that can affect the fetus.
The longer mental illness is untreated, the harder it can be to treat, and the higher the risk of chronic mental illness.
It may have a negative impact on the woman’s relationships with her partner and her other children.
The biggest risk factor for postpartum mental illness is untreated mental illness during pregnancy.
The study counters earlier research that suggested a possible link between antidepressant use in pregnancy and autism risk in children. Dr. Vigod says the new research used a more detailed approach to ensure an accurate comparison.
“The problem with those earlier studies is that for women who take antidepressant medications during pregnancy, there’s some reason why they’re taking the medication: they suffer from depression or anxiety,” she says.
That alone means there may be differences between these women and those not taking antidepressants, so a simple comparison of autism rates may be very misleading.
“It’s possible that depression or anxiety could have a direct impact on fetal brain development through physiological mechanisms,” Dr. Vigod explains. “It has been shown that depression and autism have a shared genetic predisposition. So if a woman has depression or anxiety, even if she’s not symptomatic in pregnancy, her child might have a higher risk of developing autism just by shared genetics.”
The symptoms of anxiety and depression may also have an effect on pregnancy.
“For example, if a woman has depression or anxiety she may also be more likely to not have as good nutrition, she might not be sleeping as well, she might be more likely to use alcohol or drugs, or she might have other medical conditions.”
All of those issues make it hard to isolate the possible effects of antidepressant medications from the potential effects of mental illness.
“We set out to try to balance out the groups to better understand whether this was a causal relationship or not,” Dr. Vigod says.
More accurate comparisons
To do that, she and her research colleagues used a special method called high dimensional propensity score (HDPS) analysis. This method looks for thousands of different types of health claims, from diagnoses and prescriptions to hospital stays and emergency department visits. The HDPS score of the women who took antidepressants in pregnancy was then matched to a more balanced group of women with a similar score, but who did not take antidepressants in pregnancy.
“When we did that in our main analysis, suddenly there was no longer an association between antidepressant exposure and autism,” Dr. Vigod says.
The researchers then looked at some of the results more closely.
First, they identified women who had at least two children, and who had taken antidepressants in at least one pregnancy and not in another. They compared autism risk in the siblings, and found no difference between the children exposed to antidepressants and those who weren’t.
Then, they compared the children of women who took antidepressants in pregnancy to the children of women who stopped taking antidepressants shortly before pregnancy.
“Again, in that analysis those children were not significantly different in their autism risk,” Dr. Vigod says.
These additional comparisons support the main study result: the findings showed no evidence that antidepressants in pregnancy are independently related to autism risk in children.
“What that suggests is that while kids whose moms took antidepressants may be at higher risk of autism, it’s probably not because of the antidepressants,” Dr. Vigod says.
“While we can never say that any medication exposure has zero risk, in general these medications are relatively low risk, so if women require them for their psychiatric stability, they can feel reassured that they are not unduly putting their children at risk.”
The study results may also be reassuring to mothers of children with autism who may have used antidepressants during pregnancy.
“These results may also be reassuring for those parents, to say that your child having autism isn’t a result of a decision you made,” Dr. Vigod says. “I think that can be very helpful, too.”
While women are having more children today than they were 10 years ago, according to the Pew Research Center, they're also having babies when they're older — a recent report found that 86% of U.S. females have given birth between the ages of 40 and 44, a 6% increase from 2006.
That may be why fertility is also a common issue, as the Office on Women's Health says one of the top risk factors concerning an inability to conceive is age. So it begs the question: When is a woman the most fertile?
The Facts About Fertility
Your odds of getting pregnant are highest in your 20s and 30s, as this is when women are technically the most fertile and have some of the best quality eggs, says Beth W. Rackow, M.D., associate professor of obstetrics and gynecology and pediatrics at Columbia University Medical Center. It's also when you're least likely to have to wait: According to the American College of Obstetricians and Gynecologists (ACOG), healthy couples in their 20s and 30s have a 25-30% chance of getting pregnant in a single menstrual cycle.
But around age 35, those numbers slowly and steadily dwindle, Dr. Rackow says. The risk of miscarriage also increases due to poorer egg quality. After age 37, a woman's odds of becoming pregnant decreases rapidly, ACOG says, and by the time a woman celebrates her 40th birthday, there's a less than 10% chance of getting pregnant within each menstrual cycle.
Which is why, if a woman is under the age of 35 and has been trying to get pregnant for one year, it's recommended that she receive an infertility evaluation, Dr. Rackow says. If she's between the ages of 35 and 40, only wait six months before seeing a specialist. In your 40s, it's important to seek medical attention if there are no signs of conception after only two or three cycles.
"We don't want to scare women that by age 35 they aren't going to get pregnant — that's not the case," Dr. Rackow says. "[But] it gets more difficult as a woman gets older, so we don't want them, at age 35, to be trying for two years and then see us when we could have done something sooner."
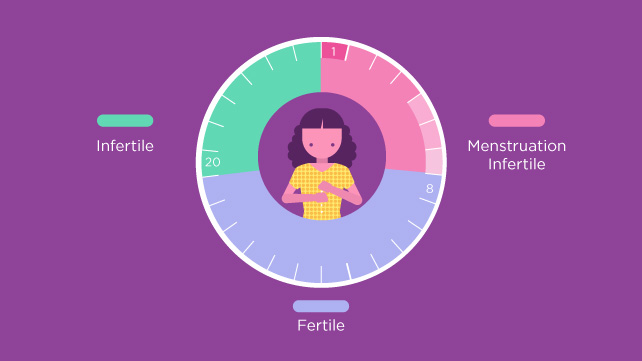
Your Fertility During Each Cycle
Making a baby the old-fashioned way comes down to figuring out when your body is ovulating. The ovulation phase, or the time in a woman's menstrual cycle in which an ovary releases an egg in order to be fertilized, lasts up to two days. There's the day of ovulation itself (AKA when the egg is released), along with the 24 hours leading up to it. That's when you're most fertile, Dr. Rackow says.
Couple that with sperm's ability to live inside the female reproductive tract for 48 to 72 hours, and your highest likelihood of success is, you guessed it, during the ovulation phase. "We encourage couples to be intimate every other day leading up to the timing of ovulation, and then every day [during the ovulation phase]," Dr. Rackow says.
As for how to pinpoint this momentous monthly occurrence, begin by tracking the length of your menstrual cycle, as some women's cycles can be 26 days and others' 32 (though the average is 28), Dr. Rackow says. Then, pay attention to when you get your period. "About 12 to 14 days before your next period is usually when you would ovulate," she says.
Your body also gives signs that you're ovulating. Clear vaginal discharge (or cervical mucus), breast tenderness, and pelvic cramping are common symptoms, Dr. Rackow says, and many women also experience a slight increase in body temperature during the ovulation phase, according to the American Pregnancy Association.
How to Tell When You're Ovulating
Other than reading the all-natural signs from your body, there are ways to tell if you're ovulating. Dr. Rackow recommends a urine ovulation kit, which measures when the body has a surge of luteinizing horrmone that signals ovulation. And while there are digital tests available, she notes that the daily test strips work just as well.
Pregmate 50 Ovulation LH Test Strips
$15.95
BUY NOW
Otherwise, a fertility app could be useful in helping you keep track of your cycle. That way you always have it on you, you can log symptoms on the fly, and you can even set up alerts to remind you when you're in the ovulation phase. (And tell your partner it's time to get busy.) Nathaniel DeNicola, M.D., assistant professor of obstetrics and gynecology at the GW School of Medicine and Health Sciences, says the ones he sees being used most frequently are Glow, Clue, and Ovia Health (formerly known as Ovuline).
Just don't rely on the apps to be the end-all, be-all source of knowledge for getting pregnant. Yes, health apps are on the rise — a recent study found that more than 70% of U.S. adults use an app to self-monitor their well-being — but Dr. DeNicola says the limited research that has been conducted to determine the accuracy of predicting the fertility window “has been a little underwhelming.”
And, whatever you do, don't forget to tell your doctor about any tests and trackers you're using when trying to conceive, Dr. DeNicola says. "A lot of what we do in fertility and achieving conception counseling is looking at the timing of periods," so your doctor will be able to use that information to get a more in-depth look at your health, potentially making it easier to spot health concerns, notice if something is irregular, or make more personalized suggestions that could result in fertility success.
Pregnancy brings with it a new set of additional responsibilities. The mother has to be extra vigilant about monitoring and caring for her health. This ensures that sufficient nutrition is being provided to the growing infant, at the same time, ensuring no harm comes to you. Listed below are some simple ways to do the same.
1. Prenatal care: As soon as you realize you are pregnant, it is advisable to talk to a doctor or a midwife about proper prenatal care. This could include anything and everything from prenatal vitamins to food habits to exercise to sleeping habits to periodic scanning and a number of other things that your doctor will prescribe.
2. Diet: You need to ensure two things that is you are eating enough for two people and everything is healthy and not harmful for the little one that gets all its nutrition through you. The diet should be healthy, nutritious, wholesome and of course free of junk. Some pointers to a healthy diet include:
a. Include a good amount of fruits and vegetables every day; break it into five small portions.
b. Sufficient amount of carbohydrates should be the basis of each meal.
c. Whole grains are preferred to white grains, which also give good amount of fiber.
d. A good amount of proteins including fish, eggs, meat, nuts, pulses, milk, and other dairy products.
e. Ensure adequate amount of iron, calcium, and other minerals are included in the diet.
f. Avoid eating unpasteurized dairy products, uncooked or undercooked food and smoked seafood.
g. While most vitamin requirements should be met through the diet, in some people, prenatal vitamins which provide the increased demands for folic acid.
3. Weight gain: If your weight was normal for your age and height before pregnancy, expect to add about 12 to 15 kg during your pregnancy. Consult with your doctor on weight changes and nutritional aspects to monitor weight throughout pregnancy. This could change based on if it is twins, your weight before pregnancy, and body type.
4. Exercise: Exercising during pregnancy is being increasingly encouraged for the following reasons:
a. Improved energy levels
b. Controls back pain
c. Improved sleep pattern
d. Improves constipation
e. Improves muscles strength and endurance.
There are specific exercises designed to benefit the pregnant women. Whether it is walking or swimming aimed at improving overall health or Kegel exercises aimed at improving vaginal and perineal muscles, your doctor should be able to draw up a routine.
5. Lifestyle changes: With pregnancy setting in, it is time to bid goodbye to smoking and drinking alcohol. Continued smoking after onset of pregnancy has many serious complications, including growth retardation, low birth weight. Alcohol can lead to miscarriage, stillbirth and premature delivery.
Seeing spots of blood during pregnancy is usually a cause for concern. However, it is not uncommon. The light bleeding, which is known as spotting may occur for a number of reasons.
Bleeding during the first trimester:
Spotting is most likely to happen during early pregnancy and the reasons could be many, such as:
1. Implantation bleeding. You may experience some normal spotting within the first six to 12 days after you conceive as the fertilized egg implants itself in the lining of the uterus. Some women don't realize they are pregnant because they mistake this bleeding for a light period. Usually, the bleeding is very light and lasts from a few hours to a few days.
2. Miscarriage. Because miscarriage is most common during the first 12 weeks of pregnancy, it tends to be one of the biggest concerns with first trimester bleeding. However, first trimester bleeding does not necessarily mean that you’ve lost the baby or going to miscarry. In fact, if a heartbeat is seen on ultrasound, over 90% of women who experience first trimester vaginal bleeding will not miscarry.
3. Molar pregnancy (also called gestational trophoblastic disease). This is a very rare condition in which abnormal tissue grows inside the uterus instead of a baby. In rare cases, the tissue is cancerous and can spread to other parts of the body. Other symptoms of molar pregnancy are severe nausea and vomiting, and rapid enlargement of the uterus.
Additional causes of bleeding in early pregnancy include:
-Cervical changes. During pregnancy, extra blood flows to the cervix. Intercourse or a Pap test, which cause contact with the cervix, can trigger bleeding. This type of bleeding isn't cause for concern.
-Infection. Any infection of the cervix, vagina, or a sexually transmitted infection (such as chlamydia, gonorrhea, or herpes) can cause bleeding in the first trimester.
Bleeding during the second or third trimesters:
Spotting may also occur during late pregnancy and the possible reasons are listed below.
1. Problems related to placenta like placenta previa placental abruption can also result in spotting. These are serious conditions when the placenta either covers the cervix or it gets detached from the uterine wall respectively.
2.Uterine rupture is the rare and unfortunate event when a scar from a previous surgery (like the removal of fibroid or previous caesarean scar bursts open and the baby slips into the pregnant woman's abdomen.
3.Premature labour occurs when your body is too eager to deliver the baby, usually one month before the due date of delivery.
4. Vasa Previa is another rare condition when a baby who is still developing has his blood vessels entangled in the umbilical cord or placenta-crossing the cervix. It is extremely dangerous because the blood vessels may burst open thus causing the baby to bleed and lose oxygen.
Investigating early bleeding
Your doctor is likely to begin with an internal examination to feel the size of your uterus and to look for any obvious visible sign of bleeding.
-Ultrasound: After about six weeks of pregnancy the baby’s heart beat can usually be seen on ultrasound. If you have been bleeding, you will likely be offered a vaginal ultrasound because it offers the best possible view of your pregnancy. A vaginal ultrasound is a narrow probe, which is put inside the vagina; it feels much like an internal examination and is quite safe.
-Blood tests: A blood test can measure the level of the pregnancy hormone hCG (human Chorionic Gonadotrophin), which changes depending on how pregnant you are.
Bottom line:
No matter when it occurs, any bleeding during pregnancy warrants a phone call to your doctor or midwife, even if only to confirm nothing is amiss. Be prepared to answer detailed questions about the color, amount, and timing of blood in order to best help your practitioner determine the possible cause.