If you like your food sweet, but worry about calories at the same time, chances are you are leaning towards artificial sweeteners to solve your dilemma. The market is flooded with artificial sweeteners, so how do you choose one? And what are their pros and cons?
Besides weight control, artificial sweeteners are also used by people suffering from diabetes. But there is a debate as to how safe artificial sweeteners are, for normal people and diabetics alike.
You get multiple choices from aspartame to sucralose, present in stores. However, it is better to be educated about their benefits and disadvantages.
The pros and cons of most popular sweeteners are as follows:
1. Saccharin: This sugar substitute has been in the market for the longest.
Pros:
a) It has zero calories
b) It does not elevate the levels of blood sugar
c) 200-700 times sweeter than normal sugar
Cons:
a) It is a possible carcinogen (substances that cause cancer)
b) There is also the danger of saccharin acting as an allergen (substance that cause allergy)
2. Aspartame: It is the most commonly used sugar substitute. Almost all the food items that boast of being sugar-free have aspartame in them.
Pros:
a) 160-220 times sweeter than common sugar
b) A small amount goes a long way, so calorie intake is lesser
Cons:
a) Headaches, depression and cancer have been linked to aspartame use
b) Increased hunger
3. Sucralose: This sugar substitute is derived from sugar itself. It is gradually becoming the most popularly used sweetener as it is found in almost all cooked or baked foods.
Pros:
a) It is heat resistant, so it is used liberally in cooking and baking
b) It has very few calories
Cons:
a) Weight gain is still possible
b) It has chlorine in it, which is a carcinogen
4. Neotame: This is a new invention and is chemically related to aspartame.
Pros:
a) 7000 -13000 times sweeter than common sugar with zero calories
b) Apparently, it is safe for consumption for teens, children and even for women who are pregnant or breastfeeding
Cons:
a) There isn't enough research done on Neotame, therefore very little is known about it
b) Since its chemical composition is closer to aspartame, there is much controversy about "neotame" affecting people the same way as aspartame.
We were talking about pre-diabetes and in this video we are going to talk about reversal of pre-diabetes. And how Dr. Monga Medi Clinic is helping people in reversing pre-diabetes stage. So, my question to you Dr. Yuvraj Monga would be how do we help people manage pre-diabetes stage? Our focus on diabetes has been there since years. And recently we have started program on pre-diabetes reversal. So, we believe that if we catch the patient early before it becomes or develop diabetes, is focused to reverse the pre-diabetes stage which is easy and more meaningful and decreases the long term morbidity of diabetes, complications of diabetes and cost and time and lifestyle quality is improved.
So, it’s a initiative which will help many many patients. As I said 10% of in India polputaion is pre-diabetics. So, prevention is better than cure. We all know that. So, this is what we are trying to achieve. Prevent patients of pre-diabetes to become diabetic. So, what we are doing is, we meet patients who are coming attendance, relatives of the patients or sometimes we are doing routine check-ups to find blood sugar or fasting level are higher towards under 10, under 16 and 20. And HbA1c is around 6, 6.2, 6.3. So, we counsel those patients to tell and that you are becoming diabetics. Your blood sugar is more than 100/26, fasting after 10 hours and HbA1c is more than 6/4. And you will become diabetic. So, we tell them that this is the stage where you are prone to become diabetic. Please put effort on you and we’ll help you.
So, we put them on the 90 days program. There we take the detailed history, their lifestyle history, their daily recall of the lifestyle. No. 2: we tell them the dietary modifications required. So, a dietitian is allocated to them. So, we plan their 7 visits on 0 day, 7 day, 15 day, 30th day, 45th day, 60the day and 90th day. So, 90 days food a lot is maintained. So we maintain their food habits. So, we tease them to reduce carbohydrates. We ask them to stop junk and maida and oily food like breads, biscuits, momos and you know butter naans, bhaturas, idaly, sambar or parathas, and reduce the carbohydrate by 70% and increase protein intake by 200%-300%. Increase protein by 300% or 3 times like increase eggs, curd, yoghurt, daal, chicken breast.
So, focus is on their food habits and monitoring sugar. At least once in 10 days, or 1 to 2 weeks. So, bring down sugar less than 10/100. And doing their HbA1c after 90 days and also focusing on lifestyle. We request them to sleep early. Waking up till 11 PM, 1 AM or 2 AM or sleep before 10:30. And thirdly, most important focus is exercise. Ask them to walk 45-60 mins per day. So, if their food habits are improved, their exercises are improved, thirdly, if their food are maintained and they are exercising, they will improve. Their sugar levels will come down. And if require we add some ayurvedic drugs. Like chadrmabhatti, madhunashtanibhatti, madhurakshak powder. So, in 90 days, we bring down their sugar levels by 122 less than 900. Target is 90 blood sugar level.
As you see less than 5.7. So, if we achieve that we are saving them from becoming diabetics. It’s a huge reduction of disease burden in the country. And we hope that the government bodies, schools, institutes and othe medical institutes focus on this. So, we can decrease the diabetic load from the country. Thank you so much. Thank you so much Dr. Yuvraj. So, we have seen that pre-diabetes can be a wake up call for you. So, get your test done ad if you think that, if the test tell that you are going to be a diabetics soon, take measure steps and come to Dr. Monga Clinic where we have patients who have reversed their pre-diabetics stage.
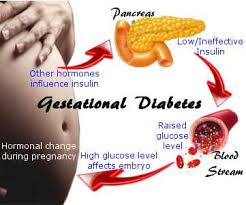
Gestational diabetes arises in certain women who cannot overcome the insulin resistance that develops during pregnancy. In most cases, the condition goes away after the baby is delivered. However, women who have gestational diabetes have increased risks of developing Type 2 diabetes later in life.
It’s important to note that gestational diabetes is not actually the cause of that long-term increased risk of Type 2 diabetes. In fact, it’s the other way around: the increased risk of Type 2 diabetes was there all along, even before pregnancy, and is the cause of the gestational diabetes.
“Gestational diabetes appears to be an early symptom of an abnormal ability to secrete insulin,” explains Dr. Lorraine Lipscombe, director of the Centre for Integrated Diabetes Care at Women’s College Hospital (WCH). “It’s an early sign of a disorder that can eventually lead to Type 2 diabetes.”
Insulin, a hormone secreted by the pancreas, regulates blood sugar levels. Abnormal insulin secretion can lead to high blood sugar, which is the main characteristic of diabetes.
Treatment for gestational diabetes protects the baby from the effects of high blood sugar and from the increased insulin production required to control it. Because insulin is a growth factor, women with gestational diabetes may have large babies, which increases the risk of delivery complications. The increased need for insulin can also stress the baby’s pancreas before birth.
“There is evidence emerging that if they are exposed to high blood sugars in pregnancy, the baby’s pancreas has to work harder and that can lead to a potential increased risk of diabetes and insulin secretory defects in the baby,” Dr. Lipscombe explains. “That’s the other concern: that over the years it predisposes the baby to a higher risk of Type 2 diabetes, so it’s a vicious cycle.”
Early warning
Gestational diabetes is treated in pregnancy to try to avoid or minimize the short- and long-term risks to the baby. For mothers, it can provide an early warning of their own health risks.
“Women get gestational diabetes because they have risk factors for Type 2 diabetes, but it hasn’t developed yet,” Dr. Lipscombe says. “As they get older, especially if they gain weight or if they have an unhealthy diet, or they have other factors that play into the increased challenge to the pancreas, then eventually the pancreas has to work harder, and eventually it fails to the point where they get Type 2 diabetes.”
While it may increase the baby’s future diabetes risk, research indicates that gestational diabetes does not add to a woman’s pre-existing risk of Type 2 diabetes.
“A number of studies have compared women who do and do not get pregnant, who have similar risk profiles,” Dr. Lipscombe says. “One group will get gestational diabetes in pregnancy and the other group won’t get it because they never got pregnant. And it appears that the pregnancy does not increase the risk further. So the gestational diabetes does not make them progress to Type 2 diabetes more rapidly.”
Although the lifetime risk of Type 2 diabetes for women with gestational diabetes may be as high as 50 per cent, it is not a certainty. Research suggests that lifestyle can play an important role in managing those risks for women who have had gestational diabetes.
Research using data from the Nurses’ Health Study II looked at the long-term health of study participants with a history of gestational diabetes.
“For the women who remained more active and kept their weight healthy, their risk of diabetes was much lower despite the gestational diabetes,” Dr. Lipscombe says. “So we know that by keeping to a healthy weight and staying physically active you can reduce your risk of Type 2 diabetes even if you had gestational diabetes. It’s not a fait accompli – you can do something about it.”
Encouraging healthy changes
That’s one of the reasons Dr. Lipscombe and her colleagues at the Women’s College Hospital Research Institute are studying a preventive program. Now in its pilot phase, it is designed to support new mothers who have had gestational diabetes to make healthy lifestyle changes. The home-based program is adapted from WCH’s highly successful Women’s Cardiovascular Health Initiative program. It includes telephone counselling and a personal health coach to help women build healthier habits to reduce their long-term risk of Type 2 diabetes.
“It’s not easy to engage new mothers to change their behaviour when they’ve just had a baby,” Dr. Lipscombe says. “We’ve trained the coaches to be sensitive to the fact that these women are in a very demanding period of their life, but it is a time when bad habits do form because of those challenges.”
There is no data from the trial yet, but it has completed recruitment. Dr. Lipscombe reports that they have received positive feedback from participants: 98 per cent would recommend the program to other mothers with gestational diabetes, and 96 per cent described their own experience in the study as good, very good or excellent.
“We’ve had over 70 women who have come back for their final assessment and many have really made positive changes and were starting to see positive results,” she says. “It’s our hope that they will sustain that long-term.”
What is Low Sex Drive?
Low sex drive, medically known as Hypoactive Sexual Desire Disorder (HSSD), is a condition where you may notice a drop in the urge to have sex or engage in any sort of sexual activity. It is something that everyone may go through at some point in their life. However, if this prolongs, you may be suffering from HSSD and you need treatment for the same. According to statistics, about 15 percent of men and 30 percent of women go through this at some point of time but never pay much heed to it.
What Causes Low Sex Drive?
The factors that contribute to low sex drive may differ in men and women.
Causes In Men
Erectile dysfunction
Alcohol and or smoking
Diabetes
Hypothyroidism
Low levels of testosterone
Obesity
Drugs dealing with depression, blood pressure, etc.
Stress and anxiety related disorders
Lost spark in marriage
Causes In Women
Childbirth
Pregnancy
Diabetes
Birth-control pills
Drugs, smoking, alcohol
Hysterectomy
Hypothyroidism
Drugs for depression, blood pressure and pain
Stress and anxiety
Traumatic incidents in childhood, such as child abuse
Symptoms of Low Libido
Low sex drive happens over a period of time. If it happens over a few days, then it is nothing of great concern. However, if the symptoms persist over a span of few weeks then you may consider treatment. If you notice the following symptoms, then it may be low sex drive:
Sex has become less frequent
Your partner points out your disinterest in sexual activities
You feel too lazy to initiate sex
If you have stopped enjoying sex altogether
Sex is less dynamic and more mechanical
There is change in your pattern of desiring sex
Aversion to sex
No arousal even after sufficient stimulation
How To Treat it with Homeopathy?
Homeopathy helps to treat the underlying disease which may be responsible for low sex drive. There are number of cases in which low sex drive may be present without any other disease in the background. Homeopathy offers promising results in improving low sex drive. It helps in following ways:
Treating the underlying cause
Treatment of Erectile dysfunction
Reducing stress and improving your stress coping system
Replacing your antidepressant and anti-anxiety medicines, whenever possible
Enhancing your moods and stimulating your sex drive
Homeopathy is strongly recommended in the cases of Low sex drive or Loss of Libido. The homeopathy drugs that can be prescribed to you for boosting your libido are:
Lycopodium clavatum
Ashwagandha
Argentum nitricum or silver nitrate
Turnera diffusa or Damiana
Women may be at greater risk for developing diabetes, heart disease and stroke in the years before menopause, rather than afterward, a U.S. study suggests. This may mean that the higher cardiovascular risk seen among post-menopausal women could be related to changes in that time before menopause and less so to the changes after menopause has occurred," said lead study author Dr. Mark DeBoer, a researcher at University of Virginia School of Medicine in Charlottesville. While the reasons for this are unclear, the findings suggest that women may need to pay especially close attention to cardiovascular risk factors in the years leading up to menopause and consider lifestyle changes like improved diet and exercise habits that can make problems like diabetes and heart disease less likely, DeBoer added by email.
Menopause typically happens between ages 45 and 55. As the ovaries curb production of estrogen and progesterone, menstruation stops, and women can experience symptoms such as hot flashes, night sweats and vaginal dryness. Certain treatments for menopause symptoms that contain man-made versions of the hormones estrogen and progestin have also been linked to an increase risk of heart attack and stroke.Previous research has also linked menopause to an increased risk of what's known as metabolic syndrome, a constellation of conditions that increase the risk of heart disease, diabetes and stroke. Obesity, inactivity and a history of smoking appear to make these problems more likely.
For the current study, researchers examined data on 1,470 white and African-American women participating in a national study of the causes and health effects of hardening of the arteries.All of the women went through menopause during the ten-year study period.Researchers focused on five things that contribute to metabolic syndrome: expanding waist circumference, elevated fats in the flood, declines in so-called "good" HDL cholesterol, spikes in blood pressure and increased levels of sugar in the blood. After taking into account whether women used hormone-replacement therapy, researchers still found bigger changes in triglycerides (fats in the blood), cholesterol and glucose (blood sugar) before menopause than afterwards.For white women, waist size spiked more after menopause, however.African-American women experienced larger increases in blood pressure after menopause than before, the researchers report in the Journal of the American Heart Association.
One limitation of the study is that researchers defined the timing of menopause based on whether women said they had a menstrual period in the previous two years, the authors note. Menopause is commonly diagnosed after women cease menstruation for one year, which means the study may have categorized some women as going through this transition who had already completed it. Researchers also lacked data on hormone levels for individual women, even though these can fluctuate and influence the risk for metabolic problems, said Dr. Robert Eckel, of the University of Colorado Anschutz Medical Campus in Aurora.
Not all types of hormone-replacement therapy carry the same risks, and the study also didn't account for the way hormones were administered, Eckel, who wasn't involved in the study, said by email. "Cardiovascular disease screening remains important for all adults including men and women," Eckel said. "Perhaps the frequency of evaluation should be more emphasized in this important peri-menopausal interval (between ages 45-55) in women - more science needed here."