Ultrasound for infertility
What is Ultrasound for infertility?
Ultrasound scans are an essential part of infertility testing and fertility treatment. If you’ve had a child before, you may be familiar with the kind of ultrasound done during mid to late pregnancy. Even if you’ve never had a child, you may have seen pregnancy ultrasound exams on movies or television. Or, perhaps, a friend or family member may have shared an ultrasound image of their unborn child with you.
Ultrasounds done during mid to late pregnancy are usually abdominal ultrasounds. In other words, a transducer (a device that emits and receives sound waves for an ultrasound) is moved around over the abdomen.
For fertility testing and treatment, the majority of ultrasounds are done transvaginally—that is to say via the vagina—with a slender specialized wand.
The ultrasounds are not painful, though they can be slightly uncomfortable.
During infertility testing, ultrasound scans can provide information on the ovaries, endometrial lining, and uterus. Specialized ultrasounds can be used to evaluate ovarian reserves, the uterine shape in more detail, and whether the fallopian tubes are open or blocked.
During fertility treatment, ultrasound is used to monitor follicle development in the ovaries and the thickness of the endometrial lining. Ultrasound is also used during IVF for egg retrieval, to guide the needle through the vaginal wall to the ovaries. Some doctors use ultrasound during embryo transfer.
If you get pregnant, your reproductive endocrinologist will likely order a few ultrasounds before transferring you back to your regular OB/GYN.
Infertility Ultrasound Scan Basics:
Ultrasound scans work by using high-frequency sound waves to create an image of your internal organs. You won’t be able to hear the sound waves.
A transducer is a device used during an ultrasound to emit and receive these high-frequency sound waves. During fertility testing and treatment, the technician is likely to use two different kinds of transducer devices: one that is used for abdominal ultrasound and a second that is used transvaginally.
During an abdominal ultrasound, a gel is squirted over your abdomen. Then, the transducer is gently moved over the abdomen. The gel makes it easier for the transducer to slide around over your skin.
During a transvaginal ultrasound, the transducer is shaped like a slender, long wand. A condom is placed over the wand and a lubricant gel is generously squirted over the condom.
The technician will hand you the handle of the transducer wand, so you can place the transducer gently inside of your vagina as far as it will comfortably go. You will then hand off the handle to the technician, who will conduct the exam.
Sound waves are emitted by the transducer. They echo (or bounce back) when they hit your internal organs. The ultrasound machine interprets these signals and turns them into a digital image.
Before an abdominal ultrasound, your doctor will likely ask you to drink several cups of water in the hours before your exam but request that you don’t relieve yourself if you feel the need to urinate. (You probably will feel the urge to go!)
A full bladder pushes your intestines out of the way, so your reproductive organs are easier to see. Once the abdominal ultrasound is finished, you’ll be able to use the bathroom.
However, to see the detail needed for fertility testing and treatment, transvaginal ultrasound provides even better imagery.
The transvaginal transducer tip is placed right below the cervix, which is closer to your reproductive organs.
Beside the abdominal and transvaginal ultrasound, there are other specialized ultrasound scans that your doctor may request.
Antral follicle count ultrasound: this is done with the usual transvaginal ultrasound device, but requires special training for the technician to complete accurately.
Antral follicle count ultrasounds can help determine your ovarian reserves and possibly help diagnosis polycystic ovarian syndrome (PCOS). You may or may not have an antral follicle count exam as part of your basic fertility workup.
This may also be scheduled separately or at the same time as a general ultrasound scan.
3D ultrasound: Most ultrasound imagery is two-dimensional. Advancing technology now can also generate three-dimensional images.
This allows for better detection of some uterine abnormalities and fallopian tube problems that are not visible on a typical 2D ultrasound scan.
Sonohysterogram: A sonohysterogram is a specialized ultrasound that involves transferring a saline solution into the uterus via a catheter. The saline solution fills your uterus, making it easier to visualize the shape and any possible adhesions within.
A sonohysterogram may be done during a basic fertility workup, but is more commonly used for specific situations.
Hysterosalpingo-contrast sonography (HyCoSy): This is similar to a sonohysterography, except a dye or a saline solution mixed with air bubbles is used to determine whether the fallopian tubes are open or blocked.
It’s more common for doctors to evaluate whether the fallopian tubes are open with an HSG, which is a specialized X-ray.
The advantages of having an HyCoSy over an HSG are that the HyCoSy may cause less discomfort than an HSG.
HyCoSy doesn’t require radiation or iodine exposure.
An HyCoSy may be done at the same time as a general ultrasound exam (which would mean one less appointment).
What Your Doctor Is Evaluating With Ultrasound?
General position and presence of the reproductive organs: Is everything that should be there present? Is everything in the correct area?
It seems like a very basic question, but some women are born without the ovaries or their uterus.
The ovaries: The ultrasound tech will look at your ovaries. She will take note of their size and shape.
She will also look for evidence of both normal and not normal cysts on the ovaries. Many small cysts that look like a pearl necklace may indicate polycystic ovarian syndrome. The presence of a larger endometrioma cyst may indicate possible endometriosis.
In rare cases, a mass that is not a cyst may be found on the ovaries.
Antral follicle count: This may be part of a general infertility ultrasound scan or may be scheduled separately. Antral follicles are a specific kind of follicle found in the ovaries. They are part of the egg/oocyte lifecycle.
A very low antral follicle count may indicate poor ovarian reserves. An unusually high antral follicle count may indicate PCOS.
The uterus: The ultrasound tech will note the uterine size, shape, and position.
If the ultrasound is 3D, it may also be possible to visualize certain uterine abnormalities, like a bicornuate or septate uterus.
The technician will also look for any indication of uterine masses, like fibroids, polyps, or an adenomyosis.
These can’t always be seen with a regular ultrasound. Further evaluation may require a sonohysterogram or a hysteroscopy.
Endometrium thickness: The lining of the uterus, the endometrium, thickens and changes as your menstrual cycle progresses.
The technician will look for healthy indications that the endometrium is at the stage it should be, based on the day of your exam.
The ultrasound tech will also measure the thickness of the endometrium. It should be thin before ovulation and thicker after ovulation.
Possibly fallopian tube problems: A basic ultrasound isn’t capable of capturing healthy fallopian tubes. However, a fallopian tube may be seen with a regular 2D ultrasound if it is swollen or filled with fluid, which can occur with a hydrosalpinx.
A basic ultrasound can’t determine if the fallopian tubes are clear and open. To evaluate whether the tubes are open or closed, your doctor will most likely order an HSG.
However, with a specialized ultrasound known as a hysterosalpingo-contrast sonography (HyCoSy), your doctor may be able to detect whether the tubes are blocked or not.
Possible evidence of adhesions: By gently pressing on the reproductive organs with the transvaginal transducer, the technician can see if the organs move freely and as they should, or if they seem to adhere to each other.
The tech may also use the ultrasound wand to gentle push at the ovaries, to see how they move around in the pelvic cavity. Ovaries that seem stuck to each other are sometimes called “kissing ovaries.”
Adhesions may prevent the reproductive organs from freely moving. Adhesions can form from a previous pelvic infection or from endometriosis.
Blood flow to reproductive organs: if your doctor is using color Doppler, the technician may be able to evaluate blood flow around a cyst or mass. This can help distinguish between a healthy cyst, an endometrial cyst (endometrioma), or an ovarian tumor.
Here’s what to expect:
Baseline ultrasound scan: Your doctor will likely tell you to call their office on the first day of your period, the month of your scheduled treatment cycle. They will want to schedule blood work and an ultrasound within the next few days.
This is known as your baseline ultrasound. The purpose is to check that there are no unusual cysts on the ovaries before starting the fertility drugs.
Sometimes, a stubborn corpus luteum cyst sticks around even after your period starts. This isn’t dangerous and will usually go away without intervention. However, treatment may be delayed in the meantime. Fertility drugs could exasperate the cyst.
(This first transvaginal ultrasound will likely occur when you're menstruating. While this can be an uncomfortable experience, it's nothing to be embarrassed about. You're not the first woman to be on her period during an ultrasound exam. This doesn't bother the ultrasound technician at all.)
Follicle growth: This is the number one monitoring focus during fertility treatment. These are all transvaginal ultrasound scans, and, depending on your treatment, you may be at the clinic every couple of days for one of these scans.
The doctor or ultrasound tech will be looking to see how many follicles are developing and how quickly they are growing. Your fertility medications may be adjusted up or down, depending on follicle growth.
Once the follicles reach a particular size, your “trigger shot” (an injection of hCG) or the egg retrieval will be scheduled.
It’s also possible that too few or too many follicles may develop.
If you’re going through IVF treatment, and few to no follicles are appearing, your cycle may be canceled.
If you’re having IUI or gonadotropin treatment, and too many follicles are growing, your cycle may be canceled to avoid the risk of having a high-order multiple pregnancy.
Endometrial thickness: The ultrasound tech will also likely measure your endometrial thickness. Based on this information, your doctor may change your fertility medication dosages.
Ultrasound-guided procedures: Not a part of monitoring, ultrasound may also be used during treatment itself.
During egg retrieval, for IVF treatment, an ultrasound-guided needle is used to retrieve eggs from the ovaries. Some doctors also use ultrasound during embryo transfer.
Tuberculin Skin Test
Tuberculosis (TB) is an illness caused by a bacterial infection. Most people infected with TB have no sign of the disease as the bacteria are sleeping or dormant. This is called TB infection (latent TB).
Some people with latent TB will develop TB disease (active TB). This can affect any part of the body but usually affects the lungs. In Australia, both active and latent TB can be treated.
What is the Tuberculin Skin Test (TST)?
The Tuberculin Skin Test (TST) is also known as the Mantoux Test. It is a skin test to detect if you have been infected with TB bacteria.
Why is it done?
The TST is done:
to find latent TB in a person who may have been exposed to someone diagnosed with active TB
to check if a person has latent TB infection before they start work at a health care facility
to check if a person has latent TB before they travel to a region where there are high rates of TB
before the BCG vaccination is given to babies over 6 months of age.
How is it done?
Tuberculin Skin Test being given by injection into forearmA small amount of purified protein taken from dead TB bacteria is injected under the top layer of the skin, on the forearm.
A sterile disposable needle and syringe is used to do this.
A small blister will appear at the site, which will disappear within 20 minutes. There may also be a small amount of blood at the needle site.
A small lump may form at the injection site over the next few days and you will need to return to your doctor or nurse 3 days later to have this assessed. The size of your lump measured in millimetres will indicate whether or not you have a latent TB infection.
What should I do before having the TST?
It is important that you tell the doctor or nurse if you:
have ever been treated for TB
have had a previous TST
have had a viral illness in the last week
have an illness that affects your immune system
take any medication, such as steroids, that affects your immune system
received any vaccinations in the past month.
How do I take care of the injection site?
Do not scratch or rub the injection site.
Leave the area open: do not cover with any dressing, cream or ointment.
If blisters develop and it causes discomfort, apply a cool compress to the area.
Continue your normal activities after having the TST including showering, swimming and sport.
What do the results mean?
The interpretation of the results depend on a number of factors, including:
whether you have had previous contact with TB
whether you have had a BCG vaccination
your age
your medical history.
Negative result:
If the lump is below a certain size, the result of the test is negative. Usually this means that you have not been infected with TB bacteria. However, if your contact with TB was very recent, you may need to have the test repeated in 8 to 12 weeks. A false negative can occur if you are unwell, have a weak immune system, or have had a recent live vaccination.
Positive result:
If the lump is above a certain size, the result of the test is positive. It means that you may have been infected with the TB bacteria. It does not mean you have TB disease (active TB).
When you are infected with TB bacteria you are not infectious and you cannot pass the bacteria onto other people. You are not sick but, at some stage in the future, you may develop TB disease. If you are told your TST is positive you may be asked to see a doctor for review.
What happens after I get the reading?
You will be given your result when you have the reading done. If the result is negative, you may be advised that no further follow up is required. You may be recommended to have a repeat test in the future depending on why the test was initially performed.
If the result is positive, you will require a chest X-ray and review by a medical officer. Some people with a latent TB will be offered medication to prevent them developing active TB. If your test is positive you may be advised not to have the test repeated.
What are the possible side effects?
The TST is a simple and safe test and side effects are uncommon. The side effects are mainly related to the size of the reaction and include swelling, redness and itchiness that may take a few weeks to clear.
Very strong reactions are uncommon but may result in a painful swelling of several centimetres in size, blistering or ulceration. This will heal with almost no scarring. The effects of the TST are localised to the site and more general reactions are extremely rare.
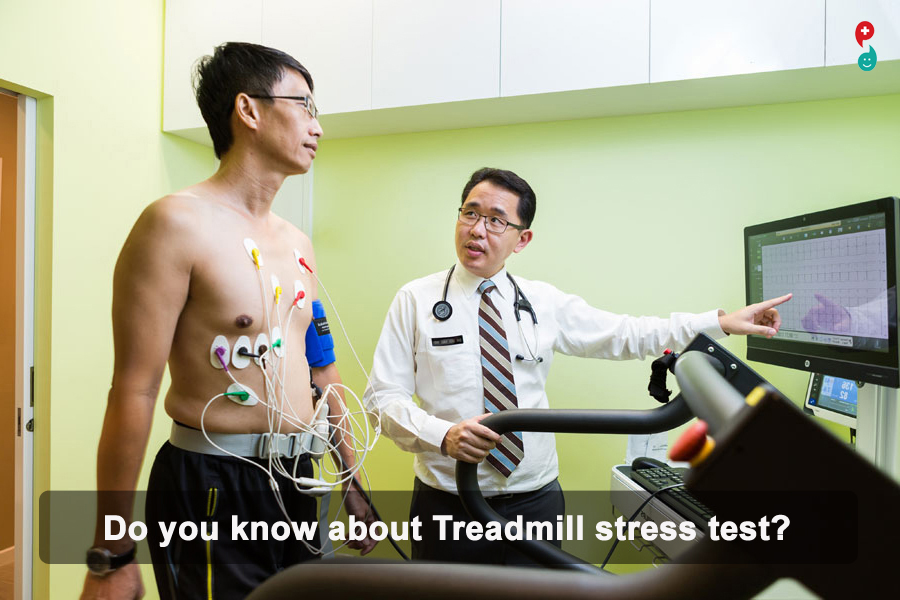
Treadmill Exercise Stress Test
(Also called: cardiac stress test, treadmill stress test)
A treadmill exercise stress test is used to determine the effects of exercise on the heart. Exercise allows doctors to detect abnormal heart rhythms (arrhythmias) and diagnose the presence or absence of coronary artery disease.
This test involves walking in place on a treadmill while monitoring the electrical activity of your heart. Throughout the test, the speed and incline of the treadmill increase. The results show how well your heart responds to the stress of different levels of exercise.
Description
A technologist will explain the test to you, take a brief medical history, and answer any questions you may have. Your blood pressure, heart rate, and electrocardiogram (ECG) will be monitored before, during, and after the test.
You will be asked to sign a consent form. This form is required before the test can proceed.
You will be asked to remove all upper body clothing, and to put on a gown with the opening to the front.
Adhesive electrodes will be put onto your chest to capture an ECG. The sites where the electrodes are placed will be cleaned with alcohol and shaved if necessary. A mild abrasion may also be used to ensure a good quality ECG recording.
Your resting blood pressure, heart rate, and ECG will be recorded.
You will be asked to walk on a treadmill. The walk starts off slowly, then the speed and incline increases at set times. It is very important that you walk as long as possible because the test is effort-dependent.
You will be monitored throughout the test. If a problem occurs, the technologist will stop the test right away. It is very important for you to tell the technologist if you experience any symptoms, such as chest pain, dizziness, unusual shortness of breath, or extreme fatigue.
Following the test, you will be asked to lie down. Your blood pressure, heart rate, and ECG will be monitored for three to five minutes after exercise.
The data will be reviewed by a cardiologist after the test is completed. A report will be sent to the doctor(s) involved in your care.
Patient Instructions
Before Your Test
For 48 hours prior to your test, stop Viagra, Cialis and Levitra.
On the Day of Your Test
For two hours prior to your test: Do not eat or drink.
Take your usual medications unless otherwise directed by your physician. Bring all of your medications with you in the original bottles.
Wear comfortable clothes and shoes that are suitable for walking on a treadmill.
After Your Test
There are no restrictions after the treadmill stress test.
What is a transvaginal ultrasound?
An ultrasound test uses high-frequency sound waves to create images of your internal organs. Imaging tests can identify abnormalities and help doctors diagnose conditions.
A transvaginal ultrasound, also called an endovaginal ultrasound, is a type of pelvic ultrasound used by doctors to examine female reproductive organs. This includes the uterus, fallopian tubes, ovaries, cervix, and vagina.
Transvaginal means through the vagina. This is an internal examination.
Unlike a regular abdominal or pelvic ultrasound, where the ultrasound wand (transducer) rests on the outside of the pelvis, this procedure involves your doctor or a technician inserting an ultrasound probe about 2 or 3 inches into your vaginal canal.
When is a transvaginal ultrasound performed?
There are many reasons why a transvaginal ultrasound might be necessary, including:
an abnormal pelvic or abdominal exam
unexplained vaginal bleeding
pelvic pain
an ectopic pregnancy (which occurs when the fetus implants outside of the uterus, usually in the fallopian tubes)
infertility
a check for cysts or uterine fibroids
verification that an IUD is placed properly
Your doctor might also recommend a transvaginal ultrasound during pregnancy to:
monitor the heartbeat of the fetus
look at the cervix for any changes that could lead to complications such as miscarriage or premature delivery
examine the placenta for abnormalities
identify the source of any abnormal bleeding
diagnose a possible miscarriage
confirm an early pregnancy
How should I prepare for a transvaginal ultrasound?
In most cases, a transvaginal ultrasound requires little preparation on your part.
Once you've arrived at your doctor's office or the hospital and you're in the examination room, you have to remove your clothes from the waist down and put on a gown.
Depending on your doctor's instructions and the reasons for the ultrasound, your bladder might need to be empty or partially full. A full bladder helps lift the intestines and allows for a clearer picture of your pelvic organs.
If your bladder needs to be full, you have to drink about 32 ounces of water or any other liquid about one hour before the procedure begins.
If you're on your menstrual cycle or if you're spotting, you have to remove any tampon you're using before the ultrasound.
What happens during a transvaginal ultrasound?
When it's time to begin the procedure, you lie down on your back on the examination table and bend your knees. There may or may not be stirrups.
Your doctor covers the ultrasound wand with a condom and lubricating gel, and then inserts it into your vagina. Make sure your provider is aware of any latex allergies you have so that a latex-free probe cover is used if necessary.
You might feel some pressure as your doctor inserts the transducer. This feeling is similar to the pressure felt during a Pap smear when your doctor inserts a speculum into your vagina.
Once the transducer is inside of you, sound waves bounce off your internal organs and transmit pictures of the inside of your pelvis onto a monitor.
The technician or doctor then slowly turns the transducer while it's still inside of your body. This provides a comprehensive picture of your organs.
Your doctor may order a saline infusion sonography (SIS). This is a special kind of transvaginal ultrasound that involves inserting sterile salt water into the uterus before the ultrasound to help identify any possible abnormalities inside the uterus.
The saline solution stretches the uterus slightly, providing a more detailed picture of the inside of the uterus than a conventional ultrasound.
Although a transvaginal ultrasound can be done on a pregnant woman or a woman with an infection, SIS cannot.
What are the risk factors with this procedure?
There are no known risk factors associated with transvaginal ultrasound.
Performing transvaginal ultrasounds on pregnant women is also safe, for both mother and fetus. This is because no radiation is used in this imaging technique.
When the transducer is inserted into your vagina, you'll feel pressure and in some cases discomfort. The discomfort should be minimal and should go away once the procedure is complete.
If something is extremely uncomfortable during the exam, be sure to let the doctor or technician know.
What do the results show?
You might get your results immediately if your doctor performs the ultrasound. If a technician performs the procedure, the images are saved and then analyzed by a radiologist. The radiologist will send the results to your doctor.
A transvaginal ultrasound helps diagnose multiple conditions, including:
cancer of the reproductive organs
routine pregnancy
cysts
fibroids
pelvic infection
ectopic pregnancy
miscarriage
placenta previa (a low-lying placenta during pregnancy that may warrant medical intervention)
Talk with your doctor about your results and what type of treatment, if any, is necessary
Testosterone is the main sex hormone (androgen) in men. It is responsible for male physical characteristics. Although it is considered to be a "male" sex hormone, it is present in the blood of both men and women. This test measures the level of testosterone in the blood.
Testosterone is mainly produced by special endocrine tissue (the Leydig cells) in the male testicles. It is also produced by the adrenal glands in both males and females and, in small amounts, by the ovaries in females.
In males, testosterone stimulates development of secondary sex characteristics, including enlargement of the penis, growth of body hair, muscle development, and a deepening voice. It is present in large amounts in males during puberty and in adult males to regulate the sex drive and maintain muscle mass. In women, testosterone is converted to estradiol, the main sex hormone in females.
Testosterone production is stimulated and controlled by luteinizing hormone (LH), which is manufactured by the pituitary gland. Testosterone works within a negative feedback mechanism: as the testosterone level increases, LH production decreases, which slows testosterone production; decreased testosterone causes increased production of LH, which in turn stimulates testosterone production.
Testosterone levels are diurnal, peaking in the early morning hours (about 4:00 to 8:00 am), with the lowest levels in the evening (about 4:00 to 8:00 pm). Levels also increase after exercise and also decrease with age.
About two-thirds of testosterone circulates in the blood bound to sex-hormone binding globulin (SHBG) and slightly less than one-third bound to albumin. A small percent (less than 4%) circulates as free testosterone. The free plus the albumin-bound testosterone is the bioavailable fraction, which can act on target tissues.
In many cases, measurement of total testosterone provides a healthcare practitioner with adequate information. However, in certain cases, for example when the level of SHBG is abnormal, a test for free or bioavailable testosterone may be performed as it may more accurately reflect the presence of a medical condition. Testosterone testing is used to diagnose several conditions in men, women, girls, and boys. Testosterone is the main sex hormone in men, produced mainly by the testicles, and is responsible for male physical characteristics. Although it is considered to be a "male" sex hormone, it is present in the blood of both males and females. (See the "What is being tested?" section for more.)
The testosterone test may be used to help evaluate conditions such as:
Delayed or precocious (early) puberty in boys
Decreased sex drive in men and women
Erectile dysfunction in men
Infertility in men and women
Testicular tumors in men
Hypothalamus or pituitary disorders
Hirsutism and virilization in girls and women
Typically, a test for total testosterone is used for diagnosis. The total testosterone test measures testosterone that is bound to proteins in the blood (e.g., albumin and sex-hormone binding globulin [SHBG]) as well as testosterone that is not bound (free testosterone).
About two-thirds of testosterone circulates in the blood bound to SHBG and slightly less than one-third bound to albumin. A small percent (less than 4%) circulates as free testosterone. Free testosterone plus the testosterone bound to albumin is the bioavailable testosterone, which can act on target tissues.
In many cases, the total testosterone test provides adequate information. However, in certain cases, for example when the level of SHBG is abnormal, a test for free or bioavailable testosterone may be performed as it may more accurately reflect the presence of a medical condition.
Depending on the reason for testing, other tests and hormone levels may be done in conjunction with testosterone testing. Some examples include:
SHBG
FSH, LH
Estrogens
DHEAS
Prolactin
17-Hydroxyprogesterone
Androstenedione
When is it ordered?
In men, the test may be ordered when infertility is suspected or when a man has a decreased sex drive or erectile dysfunction. Some other symptoms include lack of beard and body hair, decreased muscle mass, and development of breast tissue (gynecomastia). Low levels of total and bioavailable testosterone have also been associated with, or caused by, a greater presence of visceral fat (midriff or organ fat), insulin resistance, and increased risk of coronary artery disease.
In boys with delayed or slowly progressing puberty, the test is often ordered with the FSH and LH tests. Although there are differences from individual to individual as to when puberty begins, it is generally by the age of 10 years. Some symptoms of delayed puberty may include:
Delayed development of muscle mass
Lack of deepening of the voice or growth of body hair
Slow or delayed growth of testicles and penis
The test also can be ordered when a young boy seems to be undergoing a very early (precocious) puberty with obvious secondary sex characteristics. Causes of precocious puberty in boys, due to increased testosterone, include various tumors and congenital adrenal hyperplasia.
In females, testosterone testing may be done when a woman has irregular or no menstrual periods (amenorrhea), is having difficulty getting pregnant, or appears to have masculine features, such as excessive facial and body hair, male pattern baldness, and/or a low voice. Testosterone levels can rise because of tumors that develop in either the ovary or adrenal gland or because of other conditions, such as polycystic ovarian syndrome (PCOS).