A bone spur, or osteophyte, is a growth off the edge of a bone. Bone spurs most often form next to joints (where two or more bones meet). Despite the name, a bone spur is not a spiky structure, but rather a smooth outgrowth from the bone that has developed over a long period.
A bone spur, or osteophyte, is a growth off the edge of a bone. Bone spurs most often form next to joints (where 2 or more bones meet). Despite the name, a bone spur is not a spiky structure, but rather a smooth outgrowth from the bone that has developed over a long period.
Bone spurs are common as we age, and you may not even know you have them. Most bone spurs cause no signs or symptoms and often do not need to be treated. They may simply show up in tests, such as X-rays and magnetic resonance imaging (MRI) that are done for other conditions.
However, sometimes bone spurs can cause pain or loss of motion in joints. If this happens, talk to your doctor, as treatment may be needed.
What areas of the body are affected by bone spurs?
The most common problem areas for bone spurs are:
• Knees: Over time, bone spurs may cause pain, stiffness, and reduced range of motion (how far a joint can move).
• Hip: Spurs may cause pain and reduced range of motion.
• Spine: Bone spurs on the vertebrae can be a factor in the development of spinal stenosis, a narrowing of the spine in the lower back. This can pinch nerves, causing pain, numbness, and weakness in the legs.
• Shoulder: Motion in the shoulder may be affected by bone spurs rubbing against tendons and muscles in the shoulder’s rotator cuff. This can lead to tendinitis (an inflammation or irritation of a tendon) and a tear in the rotator cuff.
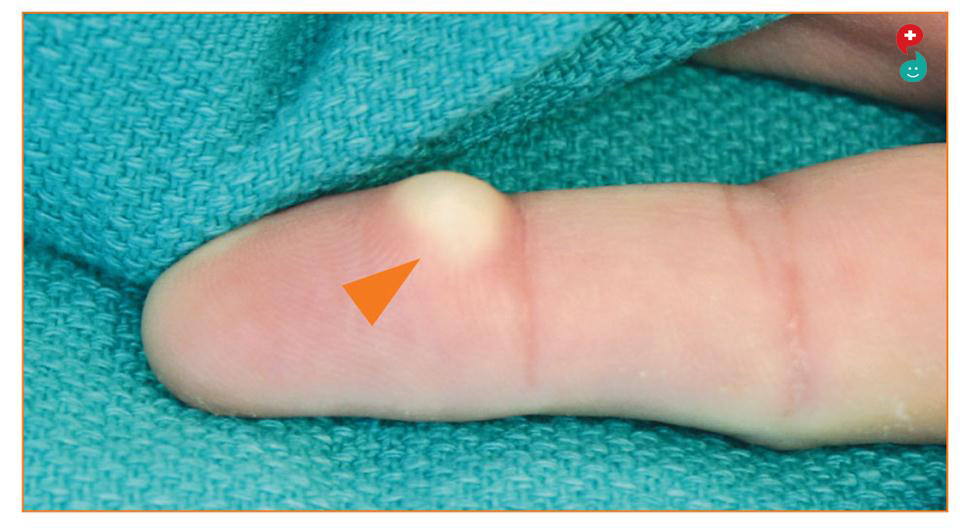
• Hands: Bone spurs can form in the finger joints. This can cause loss of motion and give the fingers a knobby appearance.
• Foot and ankle: Bone spurs may form at the back or bottom of the heel (heel spurs). They may be painful and may require shoe inserts, stretching, or, as a last resort, surgery. Bone spurs are also common in the mid-foot and great toe. Inserts and changes in shoes are the treatments before surgery is considered.
What causes bone spurs?
Bone spurs are most often caused by osteoarthritis, the most common form of arthritis. Osteoarthritis, also called degenerative joint disease, affects people over the age of 65 most often.
As we age, cartilage (the firm rubbery substance that is a cushion between bones and allows joint motion) breaks down. The result can be pain, swelling, and difficulty moving the joints. As time goes on, bone can break down, too. In response, the body develops bone growths (or spurs) near the damage.
What are the symptoms of bone spurs?
Depending on their location, bone spurs can lead to:
• Pain
• Swelling Pain
• Loss of motion in joints
• Weakness and numbness
• Tendon tears (such as rotator cuff tears)
Bone cancer describes a malignant tumor of the bone that destroys healthy bone tissue.
Bone cancer is divided into primary and secondary bone cancer: primary bone cancer forms in the cells of the bone and secondary bone cancer starts elsewhere, eventually spreading to bones.
In this article, we will discuss the survival rates, types, causes, symptoms, and treatments for bone cancer.
Fast facts on bone cancer:
Benign bone tumors are more common than malignant bone tumors.
There are a number of different bone cancer types.
Early symptoms might include pain in the affected area.
A range of diagnostic tests can help diagnose bone cancer.
Radiotherapy, chemotherapy, and surgery can all be used to treat bone cancer.
Treatment
The type of treatment for bone cancer depends on several factors, including:
the type of bone cancer
where it is located
how aggressive it is
whether it is localized or has spread
There are three approaches to treating bone cancer. These are surgery, radiation therapy, and chemotherapy.
Surgery
Surgery aims to remove the tumor and some of the bone tissue that surrounds it. If some of the cancer is left behind, it may continue to grow and eventually spread.
Limb-sparing surgery, also known as limb salvage surgery, means that surgical intervention occurs without having to amputate the limb. The surgeon may take some bone from another part of the body to replace lost bone, or an artificial bone may be fitted.
In some cases, however, amputation of a limb may be necessary.
Radiation therapy
Radiotherapy is commonly used in the treatment of many cancer types. It involves the use of high-energy X-rays or particles to destroy cancer cells. Radiotherapy works by damaging the DNA inside the tumor cells, preventing them from reproducing.
Radiotherapy can be used to:
cure the patient by completely destroying the tumor.
relieve pain in more advanced cancers.
shrink the tumor, making it easier to then surgically remove it.
eliminate the cancer cells that remained behind after surgery.
Combination therapy is radiotherapy combined with another type of therapy. This may be more effective in some cases.
Chemoradiation, or radiotherapy combined with chemotherapy, may also be used.
Chemotherapy
Chemotherapy involves the use of chemicals to treat disease. More specifically, it refers to the destruction of cancer cells. Chemotherapy has five possible goals:
Total remission: Chemotherapy aims to cure the patient. In some cases, chemotherapy alone can get rid of the cancer completely.
Combination therapy: Chemotherapy can help other therapies, such as radiotherapy or surgery, produce better results.
Delay or prevent recurrence: Chemotherapy, when used to prevent the return of cancer, is most often used after a tumor has been removed surgically.
Slow down cancer progression: Chemotherapy can slow down the advancement of the cancer.
Chemotherapy may also help to relieve symptoms; this is more frequently used for patients with advanced cancer.
Causes
While doctors are unsure or precise causes, patients with long-term inflammatory diseases, such as Paget's disease are at a significantly higher risk of developing bone cancer later in life. However, nobody can explain why one person gets bone cancer while another one does not. It is not contagious.
The following groups of people may be at a higher risk of developing bone cancer:
children or young adults aged up to 20 years
people who have received radiation therapy
individuals with a history of Paget's disease
people with a close relative who has bone cancer
individuals with hereditary retinoblastoma, a type of eye cancer that most commonly affects very young children
people with Li-Fraumeni syndrome, a rare genetic condition
Symptoms
The patient initially experiences pain in the affected area. Over time, the pain gets worse and continuous. In some cases, the pain is subtle, and the patient may not see a doctor for several months.
The progression of pain with Ewing sarcoma tends to be faster than in most other bone cancers. Typically, bone cancer pain is deep, nagging, and has a permanent character. Other symptoms include:
swelling in the affected area
weakened bones that resulting in a significantly higher risk of fracture
unintentional weight loss
a lump in the affected area
Although much less common, the patient might also experience fever, chills, and night sweats.
Australian researchers are working with an international team to understand the relationship between sitting for long periods and bone health. Sitting for long periods may be bad for your bones, with Australian researchers contributing to a global study to explore links to osteoporosis.
"In everyday life, long periods of immobility such as this are rare however, sedentary lifestyles are commonplace in modern society, through transport, work and leisure.
"If the proof of concept study identifies a significant effect of sedentary behaviour on bone metabolism, promoting frequent breaks from sitting could be a possible, and simple, preventative intervention for osteoporosis in later life."
The study will use data and blood samples already collected - but yet to be analysed - in previous sedentary behaviour studies by the research group.
About 1.2 million Australians are estimated to have osteoporosis while 6.3 million fellow residents have low bone density, the institute states.
The institute's Professor David Dunstan also added the study would shed light on the mechanisms behind osteoporosis and give a greater understanding of the relationship between lifestyle and bone health.
Experts at the Baker Heart and Diabetes Institute in Melbourne have teamed up with researchers in the United Kingdom to find out if breaking up sedentary behaviour could reverse or slow down any potential damage of the disease."We know that in extreme environments, such as total bed rest, bone loss is very high," the institute's Professor Neville Owen said in a statement on Thursday.
Bones are similar to a porous framework which is filled with minerals that make it hard and strong. With age, there is gradual degradation and the mineralized portion is lost, thereby leading to thinning of the bone. The word osteoporosis literally translates to porous bones, which is due to the gradual demineralisation. In addition to the natural ageing process, there are other diseases that can accelerate the demineralization process.
Women are more prone to demineralisation, and after the age of 40, they should take extra precaution to slow down the onset of the condition. The following are some ways to improve bone health and halt osteoporosis in the long run-
Diet: Ensure that your diet has sufficient amounts of vitamin D and calcium. Though calcium is the essential mineral for bone formation, vitamin D is required for the absorption of calcium, and therefore both these elements play a vital role in maintaining the quality of the bones in our body. Most people require about 1,000 mg of calcium and about 500 units of vitamin D for optimal bone health. This requirement goes up slightly in postmenopausal women.
Sun Exposure: In most people, exposure to the sun allows the body to make vitamin D, but careful sun protection prevents this from happening. Also, with age, the body’s ability to form intrinsic vitamin D also declines. The body, therefore, relies on supplements. Most dairy products are good sources of calcium. In addition, spinach, salmon, turnips, and broccoli are some calcium-rich foods. Supplements of calcium carbonate or calcium citrate can be taken if your diet is lacking in calcium. Vitamin D also should be included in the supplementation. The treatment for osteoporosis is incomplete without these two supplements.
Exercise With Weights: The constructive tension that exercise puts on the body helps in bone building, whatever the age may be, which prevents the onset of osteoporosis. Any exercise which improves muscle mass strengthens the bones, and puts stress on the bones is advisable. Since the fractured area due to osteoporosis mainly includes the spine, lower back exercises, yoga, tai chi, and abdominal exercises all work wonders. Pick any of these and do them for 30 minutes three times a week.
Quit Smoking: Continuing to smoke while taking osteoporosis medications is completely useless. Nicotine negates all the effects which defeat the purpose of taking the medication and is as good as taking no medication at all. So if you want the bone thinning to stop, stop smoking.
Alcohol Consumption: While a drink or two per week is permissible, more than this can harm the bones significantly.
Constant Health Watch: Talk to a doctor about how other routine medications (if any) can affect your bone health. Also, identify how frequently you should check your bone mineral density and stick to the schedule.
Bone health and osteoporosis can be managed with some conscious efforts.
Did you know: Osteoporosis causes more than 8.9 million fractures annually across the world, resulting in an osteoporotic fracture every 3 seconds?
Dr. Manoj K. Ahuja, Fortis Hospital says, “Osteoporosis literally means porous bones. It is a disease wherein the density and quality of bones are reduced. As the bones become more fragile and porous, the risk of fracture increases. The loss of bone occurs progressively, and yet silently. More often than not, there are no symptoms until the first fracture occurs”.
“For people suffering from osteoporosis, bone loss outpaces the growth of new bone. Bones become brittle, porous and prone to fracture”, says Dr. Supriya Bali, Internal Medicine, Max Hospital, Saket. So, what causes osteoporosis?
Osteoporosis is associated with a set of factors including depletion in bone mass and density as a result of ageing, previous injuries, genetic inheritance, family history of osteoporosis, and arthritis. Women (especially those who have hit menopause) are more susceptible to this condition, as they often fall prey to the deficiency of calcium and vitamin D.
“Worldwide, 1 in 3 women over the age of 50 will experience osteoporotic fractures, as will 1 in 5 men aged over 50. Osteoporosis is estimated to affect 200 million women worldwide - approximately one-tenth of women aged 60, one-fifth of women aged 70, two-fifths of women aged 80 and two-thirds of women aged 90. Overall, 61% of osteoporotic fractures occur in women, with a female-to-male ratio of 1.6”, according to the International Osteoporosis Foundation.
The Role of Nutrition in Osteoporosis
Nutrition and osteoporosis are closely linked. Thus, it is important to learn about the foods that are rich in vitamin D, calcium and other nutrients to boost your bone health. “Good nutrition is also an important part of a successful rehabilitation program in patients who have had an osteoporotic fracture”, according to the International Osteoporosis Foundation.
“The food that you eat affects your bones, so you must make healthier food choices every day and eat a well-balanced diet with plenty of dairy, fish, fruits and vegetables to get enough of the nutrients your body needs”, says Dr. Manoj K. Ahuja, Fortis Hospital.
What Should You Eat?
According to the National Osteoporosis Foundation, you must eat dairy product such as low-fat and non-fat milk, yogurt and cheese, fatty varieties of fish such as salmon, mackerel, tuna and sardines, fruits and vegetables including collard greens, turnip greens, kale, okra, brussels sprouts, Chinese cabbage, dandelion greens, mustard greens, broccoli, spinach, beet greens, artichokes, plantains, potatoes, sweet potatoes, papaya, oranges, bananas, pineapples, papaya, prunes, red peppers, green peppers, grapefruits, strawberries and papaya. Recent research has also found that olive oil, soy beans, blueberries and foods rich in omega-3s such as fish oil and flaxseed oil may also have bone boosting benefits.
Foods That Can Lead to Bone Loss
The following foods can cause your body to lose calcium and result in bone loss, according to the National Osteoporosis Foundation:
1. Alcohol: Drinking heavily can lead to bone loss.
2. Caffeine: Coffee, tea and colas may decrease calcium absorption and contribute to bone loss.
3. Beans (Legumes): While pinto beans, navy beans and peas contain calcium, they are also high in substances called phytates which interfere with your body’s ability to absorb the calcium present in beans. Tip: To reduce the phytate level, soak beans in water for several hours and then cook them in fresh water.
4. Wheat Bran: Like beans, wheat bran contains high levels of phytates as well. But unlike beans, 100% wheat bran is the only food that appears to reduce the absorption of calcium in other foods eaten at the same time. For instance, if you have milk and 100% wheat bran cereal together, your body can absorb some, but not all, of the calcium from the milk. However, the wheat bran in other foods like bread is much less concentrated and does not have a noticeable impact on calcium absorption.
5. Salty Foods: Eating foods that have a lot of salt (sodium) causes your body to lose calcium. So limit the amount of processed foods, canned foods and salt intake each day.
6. Meat and Other High Protein Foods: It’s important to get enough protein, but not too much. Many older adults do not get enough protein in their diets and this may be harmful to their bones. However, special high protein diets which contain multiple servings of meat and protein can also cause the body to lose calcium. You can make up for this loss by getting enough calcium from dairy products as they are high in protein, but also contain calcium which is important for healthy bones.