Thrombophlebitis (throm-boe-fluh-BY-tis) is an inflammatory process that causes a blood clot to form and block one or more veins, usually in your legs. The affected vein might be near the surface of your skin (superficial thrombophlebitis) or deep within a muscle (deep vein thrombosis, or DVT). Causes include trauma, surgery or prolonged inactivity.
DVT increases your risk of serious health problems. It's usually treated with blood-thinning medications. Superficial thrombophlebitis is sometimes treated with blood-thinning medications, too.
Symptoms
Superficial thrombophlebitis signs and symptoms include:
Warmth, tenderness and pain in the affected area
Redness and swelling
Deep vein thrombosis signs and symptoms include:
Pain
Swelling
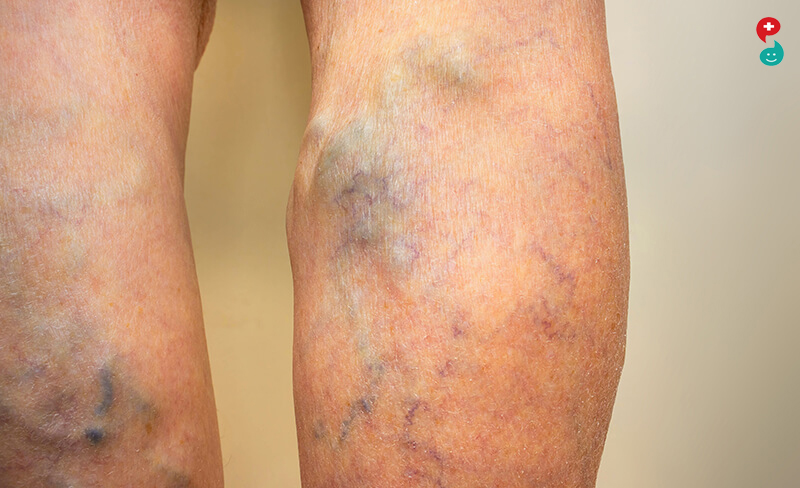
When a vein close to the surface of your skin is affected, you might see a red, hard cord just under the surface of your skin that's tender to the touch. When a deep vein in the leg is affected, your leg may become swollen, tender and painful.
When to see a doctor
See your doctor right away if you have a red, swollen or tender vein — especially if you have one or more risk factors for thrombophlebitis.
If you have leg swelling and pain and develop shortness of breath or chest pain that worsens when you breathe, go to an emergency room. These might indicate that you have a dislodged blood clot traveling through your veins to your lungs (pulmonary embolism).
Causes
The cause of thrombophlebitis is a blood clot, which can form in your blood as a result of:
An injury to a vein
An inherited blood-clotting disorder
Being immobile for long periods, such as during an injury or a hospital stay
Risk factors
Your risk of thrombophlebitis increases if you:
Are inactive for a prolonged period, either because you're confined to bed or are traveling in a car or plane for a long period
Have varicose veins, which are a common cause of superficial thrombophlebitis
Have a pacemaker or have a thin, flexible tube (catheter) in a central vein, for treatment of a medical condition, which may irritate the blood vessel wall and decrease blood flow
Are pregnant or have just given birth
Use birth control pills or hormone replacement therapy, which can make your blood more likely to clot
Have a family history of a blood-clotting disorder or a tendency to form blood clots
Have had previous episodes of thrombophlebitis
Have had a stroke
Are older than 60
Are overweight or obese
Have cancer
Smoke
If you have one or more risk factors, discuss prevention strategies with your doctor before taking long flights or road trips or if you're planning to have elective surgery, recovery from which will require you not to move much.
Complications
Complications from superficial thrombophlebitis are rare. However, if you develop DVT, the risk of serious complications increases. Complications might include:
Pulmonary embolism. If part of a deep vein clot becomes dislodged, it can travel to your lungs, where it can block an artery (embolism) and become potentially life-threatening.
Post-phlebetic syndrome. This condition, also known as post-thrombotic syndrome, can develop months or even years after you've had DVT. Post-phlebetic syndrome can cause lasting and possibly disabling pain, swelling and a feeling of heaviness in the affected leg.
Prevention
Sitting during a long flight or car ride can cause your ankles and calves to swell and increases your risk of thrombophlebitis. To help prevent a blood clot:
Take a walk. If you're flying or riding a train or bus, walk up and down the aisle once an hour or so. If you're driving, stop every hour or so and move around.
Move your legs regularly. Flex your ankles, or carefully press your feet against the floor or footrest in front of you at least 10 times each hour.
Wear loose clothing.
Drink plenty of nonalcoholic fluids to avoid dehydration.
What is a bleeding disorder?
A bleeding disorder is a condition that affects the way your blood normally clots. The clotting process, also known as coagulation, changes blood from a liquid to a solid. When you’re injured, your blood normally begins to clot to prevent a massive loss of blood. Sometimes, certain conditions prevent blood from clotting properly, which can result in heavy or prolonged bleeding.
Bleeding disorders can cause abnormal bleeding both outside and inside the body. Some disorders can drastically increase the amount of blood leaving your body. Others cause bleeding to occur under the skin or in vital organs, such as the brain
What causes a bleeding disorder?
Bleeding disorders often develop when the blood can’t clot properly. For blood to clot, your body needs blood proteins called clotting factors and blood cells called platelets. Normally, platelets clump together to form a plug at the site of a damaged or injured blood vessel. The clotting factors then come together to form a fibrin clot. This keeps the platelets in place and prevents blood from flowing out of the blood vessel.
In people with bleeding disorders, however, the clotting factors or platelets don’t work the way they should or are in short supply. When the blood doesn’t clot, excessive or prolonged bleeding can occur. It can also lead to spontaneous or sudden bleeding in the muscles, joints, or other parts of the body.
The majority of bleeding disorders are inherited, which means they’re passed from a parent to their child. However, some disorders may develop as a result of other medical conditions, such as liver disease.
Bleeding disorders may also be caused by
a low red blood cell count
a vitamin K deficiency
side effects from certain medications
Medications that can interfere with the clotting of the blood are called anticoagulants.
Types of bleeding disorders
Bleeding disorders can be inherited or acquired. Inherited disorders are passed down through genetics. Acquired disorders can develop or spontaneously occur later in life. Some bleeding disorders can result in severe bleeding following an accident or injury. In other disorders, heavy bleeding can happen suddenly and for no reason.
There are numerous different bleeding disorders, but the following are the most common ones:
Hemophilia A and B are conditions that occur when there are low levels of clotting factors in your blood. It causes heavy or unusual bleeding into the joints. Though hemophilia is rare, it can have life-threatening complications.
Factor II, V, VII, X, or XII deficiencies are bleeding disorders related to blood clotting problems or abnormal bleeding problems.
Von Willebrand's disease isthe most common inherited bleeding disorder. It develops when the blood lacks von Willebrand factor, which helps the blood to clot.
What are the symptoms of a bleeding disorder?
The symptoms can vary depending on the specific type of bleeding disorder. However, the main signs include:
unexplained and easy bruising
heavy menstrual bleeding
frequent nosebleeds
excessive bleeding from small cuts or an injury
bleeding into joints
Schedule an appointment with your doctor right away if you have one or more of these symptoms. Your doctor can diagnose your condition and help to prevent complications associated with certain blood disorders
How is a bleeding disorder diagnosed?
To diagnose a bleeding disorder, your doctor will ask you about your symptoms and medical history. They will also perform a physical examination. During your appointment, make sure to mention:
any medical conditions you currently have
any medications or supplements you may be taking
any recent falls or trauma
how often you experience the bleeding
how long the bleeding lasts
what you were doing before the bleeding began
After gathering this information, your doctor will run blood tests to make a proper diagnosis. These tests may include:
a complete blood count (CBC), which measures the amount of red and white blood cells in your body
a platelet aggregation test, which checks how well your platelets clump together
a bleeding time test, which determines how quickly your blood clots to prevent bleeding
How are bleeding disorders treated?
Treatment options vary depending on the type of bleeding disorder and its severity. Though treatments can’t cure bleeding disorders, they can help relieve the symptoms associated with certain disorders.
Iron supplementation
Your doctor may prescribe iron supplements to replenish the amount of iron in your body if you have significant blood loss. A low iron level can result in iron deficiency anemia. This condition can make you feel weak, tired, and dizzy. You may need a blood transfusion if symptoms don’t improve with iron supplementation.
Blood transfusion
A blood transfusion replaces any lost blood with blood taken from a donor. The donor blood has to match your blood type to prevent complications. This procedure can only be done in the hospital.
Other treatments
Some bleeding disorders may be treated with topical products or nasal sprays. Other disorders, including hemophilia, can be treated with factor replacement therapy. This involves injecting clotting factor concentrates into your bloodstream. These injections can prevent or control excessive bleeding.
You can also get fresh frozen plasma transfusions if you lack certain clotting factors. Fresh frozen plasma contains factors V and VIII, which are two important proteins that help with blood clotting. These transfusions must be done in a hospital.

Did you know that there are certain foods that we can eat to improve our blood circulation and prevent many heart diseases? Yes, that's right! There are many blood thinning foods that are known to reduce the risk of clotting. But, before we talk about the variety of natural blood thinning foods, it is imperative to understand what blood clotting is and how it affects our body?
Blood clotting is a normal yet complex process which is known to prevent bleeding when there is an injury or a cut in our body. However, there are times when blood clots form in some critical parts of our body like heart, lung or brain, which if not treated in time, can cause serious complications. These clots may occur in the arterial or venous blood vessels. It is when this clot breaks and travels through the blood, it disrupts the flow of blood to important organs such as heart, lungs or brain, and can result in stroke.
Here are 5 natural blood thinners to reduce blood clots and the risk of stroke:
1. Ginger
One of the best ways to add ginger to your diet is to begin your morning with tasty ginger tea. Research says that sipping ginger tea is quite beneficial and may cure many health problems. And, when it comes to blood thinning, ginger is known to reduce inflammation and further relaxes the muscles. Who knew that a single cup of ginger tea can do wonders for your health.
2. Cayenne Peppers
Cayenne peppers are power-packed with properties that help in thinning our blood. And, the credit goes to salicylates, which are found in high amount in cayenne peppers. Adding cayenne peppers to our daily diet, in the form of capsules or in the food, could lower your blood pressure and increase circulation.
3. Salmon
It is said that foods that are high in omega-3 fatty acids such as salmon, tuna and trout are one of the best blood thinning foods. It is mainly because omega-3 fatty acids help lower the cholesterol levels in our body. Moreover, they are known to reduce the chances of clotting in the blood.
4. Red Wine
Many experts and nutritionists believe that drinking a glass of red wine every day may help prevent heart diseases, as red wine is known to have properties that help in thinning the blood and further preventing clogged arteries. And, we know how much you fancy drinking red wine, so don't just get carried away and stick to only one glass a day!
5. Cinnamon
We add cinnamon to enhance the taste and fragrance of our dish or drink, especially when added to tea, it tastes bliss. But, did you know that it is a powerful anti-coagulant? Cinnamon is capable of lowering blood pressure and relieving inflammatory conditions. This may reduce the chances of having a stroke. However, long-term consumption of cinnamon may cause liver damage, therefore, make sure you use this spice sparingly.
Other than the natural foods and drinks mentioned above, there are other natural foods like pineapple, ginseng, kelp, olive oil, almonds and more that are known to reduce blood clotting. However, it's important to note that these foods need be taken in moderation. Always speak to your doctor before trying anything that could have an impact on your health.

Taking oral drugs daily can be an effective treatment for nearly 10 million cancer patients worldwide suffering from a deadly blood clot condition, results from a clinical trial have showed. People with cancer have an increased risk of developing blood clots, with roughly one in five experiencing venous thromboembolism (VTE) -- either a blood clot in a deep vein or a condition in which one or more arteries in the lungs become blocked by a blood clot.
The results from the clinical trial called “select-d” suggested that prescribing the oral drug rivaroxaban significantly reduced VTE recurrence among patients with cancer. “Clinicians were already adopting the oral drug into practice for non-cancer patients and now they have data from this study to indicate that this form of treatment is an alternative option for many cancer patients who have a clot,” said lead author Annie Young, Professor at University of Warwick in the Britain.
Although there are many causes and risk factors for VTE, cancer patients are particularly at risk due to a combination of factors such as immobility, pancreatic and gastric tumours as well as chemotherapy, the researcher said.
For the “select-d” trial, researchers enrolled 406 patients who had cancer and VTE; most (69 per cent) were receiving cancer treatment (typically chemotherapy) at the time of their VTE. Half were randomly assigned to receive low-molecular-weight heparin (dalteparin) and half were given the oral drug rivaroxaban. After six months of treatment, the VTE recurrence rate was four per cent among those taking the tablet and 11% in those receiving dalteparin. The results for secondary outcomes were mixed, the researcher said.
In patients receiving rivaroxaban, there were around the same percentage of major bleeding events (6%) as those receiving dalteparin (4 per cent) but a marked and significant increase in clinically relevant non-major bleeds (13%) with rivaroxaban compared to those having low molecular weight heparin (4%).
The reason for increased bleeding is not known. It may be because rivaroxaban is more ‘potent’, the paper published in the Journal of Clinical Oncology said.
A drug to treat bleeding may benefit some stroke patients as well, according to a study. The research, led by experts at The University of Nottingham, found that giving tranexamic acid (TXA) to people who had experienced intracerebral haemorrhage reduced the number of deaths in the early days following the stroke.
It also found that both the amount of bleeding in the brain and number of associated serious complications were lower in the patients who had received the TXA treatment.
However, the trial found no difference in the number of people who were left disabled or had died at three months after their stroke (the study’s primary outcome). The researchers believe further study is needed on larger groups of patients to enable them to fully understand the potential benefits. Nikola Sprigg, who led the trial, said, “Tranexamic acid is cheap and widely available so has the potential for reducing death and disability across the world.”
“While we failed to show significant benefits three months after stroke, the reduction in early deaths, amount of bleeding on the brain and serious complications are signs that this drug may be of benefit in the future. More trials are needed, particularly focusing on giving treatment as soon as possible after the start of bleeding in this emergency condition.
“TICH-2 cements the position of the NIHR and the UK as key players in the world of stroke research. A study of this scale would simply not have been possible without support of the NIHR infrastructure. Alongside the large stroke centres, the contribution made by the network of smaller sites across the UK has been crucial to the success of TICH-2.”
15 per cent of all strokes -- affecting around 22,000 people every year -- are caused by haemorrhagic stroke when a blood vessel in the brain bursts, leading to permanent damage. While all people with acute stroke benefit from treatment on a stroke unit, there is currently no specific treatment for haemorrhagic stroke and unfortunately many people affected will die within a few days. Those who do survive are often left with debilitating disabilities including paralysis and an inability to speak.
The five-year TICH-2 trial recruited more than 2,000 patients from 124 hospitals in 12 countries between 2013 and 2017. They were randomly sorted into two patient groups - one received TXA within eight hours of their stroke and another was given a saline placebo. In the UK, more than 80 hospitals took part in the study with support from the NIHR clinical research network. CT scans of the patients’ brains were performed 24 hours after their stroke and their progress was monitored and measured at day two and day seven after their stroke. The final follow up was performed at 90 days.
The study revealed that TXA did not improve the outcome for patients after 90 days as there was no significant difference in the number of patients who had subsequently died or had been left with disabilities between the TXA and placebo groups at three months.
However, in the TXA group there were fewer deaths by day seven following the stroke and, at day two, fewer people on TXA experienced a worsening of the bleed on their brain and had smaller amounts of blood in the brain compared to their control group counterparts.
Also, the number of patients who experienced associated serious complications (such as pneumonia and brain swelling) were lower in the patients who had received the TXA treatment compared to those who had control. The trial also found evidence that TXA might be more effective in patients with lower blood pressure as those with blood pressure lower than 170 mmHg had a more favourable outcome that those with 170mmHg and above.
Other studies have confirmed that the sooner TXA is given, the more effective it is, and ideally it needs to be given within less than 3 hours of bleeding onset. In this study only one third of patients were given treatment within 3 hours of stroke onset. As a result, the researchers have highlighted the need for further studies to find out whether giving an earlier dose of TXA might be beneficial for patients.